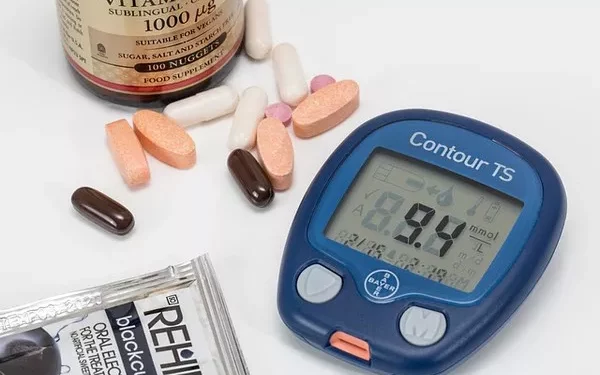
Prediabetes is a critical stage in the progression towards type 2 diabetes, characterized by elevated blood glucose levels that are higher than normal but not yet high enough to be classified as diabetes. Managing prediabetes effectively can prevent or delay the onset of type 2 diabetes and its associated complications. While lifestyle modifications such as diet and exercise are foundational in managing prediabetes, medications can also play a significant role. This article explores the medications available for prediabetes, their mechanisms, effectiveness, and considerations for their use.
Understanding Prediabetes
Prediabetes is a condition where blood glucose levels are higher than normal but not high enough to meet the criteria for type 2 diabetes. It is often asymptomatic, making it a silent risk factor for developing type 2 diabetes and cardiovascular disease. The primary goal of managing prediabetes is to reduce blood glucose levels to a normal range and to mitigate the risk of progressing to type 2 diabetes.
Diagnosis and Risk Factors
Prediabetes is diagnosed through several tests, including fasting blood glucose tests, oral glucose tolerance tests, and hemoglobin A1c tests. Elevated results in any of these tests can indicate prediabetes. Risk factors for prediabetes include obesity, sedentary lifestyle, age, family history of diabetes, and certain ethnicities.
Lifestyle Modifications
Before discussing medications, it’s important to emphasize that lifestyle changes are the cornerstone of managing prediabetes. These include:
Dietary Changes: A diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats can help regulate blood glucose levels.
Physical Activity: Regular exercise helps improve insulin sensitivity and lower blood glucose levels.
Weight Management: Losing even a modest amount of weight can significantly improve insulin resistance and blood glucose control.
Despite these interventions, some individuals may require medications to achieve optimal glucose control. This is particularly true for those who have not been able to achieve significant results through lifestyle changes alone.
Medications for Prediabetes
Several medications are used to manage prediabetes, each with its own mechanism of action, benefits, and potential side effects. The choice of medication depends on individual patient factors, including the presence of other health conditions, risk factors, and the potential for medication-related side effects.
Metformin
Metformin is the most commonly prescribed medication for prediabetes. It is a biguanide class medication that works primarily by decreasing glucose production in the liver and improving insulin sensitivity in peripheral tissues.
Mechanism of Action: Metformin lowers blood glucose levels by reducing hepatic glucose production and enhancing insulin sensitivity. It does not cause increased insulin secretion from the pancreas.
Effectiveness: Studies have shown that metformin can reduce the risk of progression from prediabetes to type 2 diabetes by approximately 30-40%. It is particularly beneficial for individuals who are overweight or obese.
Side Effects: Common side effects include gastrointestinal issues such as nausea, diarrhea, and abdominal discomfort. These side effects are often transient and can be managed by starting with a low dose and gradually increasing it.
Considerations: Metformin is generally well-tolerated and is often the first-line medication for managing prediabetes. It is not recommended for individuals with severe renal impairment due to the risk of lactic acidosis.
Thiazolidinediones (TZDs)
Thiazolidinediones, such as pioglitazone and rosiglitazone, are another class of medications used to improve insulin sensitivity. They act on the peroxisome proliferator-activated receptor-gamma (PPAR-gamma) to enhance glucose uptake in muscle and fat tissues.
Mechanism of Action: TZDs increase insulin sensitivity in peripheral tissues and decrease insulin resistance. They also have beneficial effects on lipid profiles.
Effectiveness: TZDs can be effective in lowering blood glucose levels and improving insulin sensitivity. However, their use in prediabetes is less common compared to metformin due to potential side effects.
Side Effects: TZDs may cause weight gain, fluid retention, and an increased risk of heart failure. Long-term use has also been associated with bone loss.
Considerations: TZDs are usually reserved for cases where metformin is not suitable or in combination with other medications. They should be used cautiously in individuals with a history of heart failure or significant fluid retention.
Alpha-Glucosidase Inhibitors
Alpha-glucosidase inhibitors, such as acarbose and miglitol, work by slowing down the digestion of carbohydrates in the intestines, which helps prevent postprandial (after-meal) blood glucose spikes.
Mechanism of Action: These medications inhibit enzymes in the small intestine that break down carbohydrates, resulting in slower glucose absorption and reduced postprandial blood glucose levels.
Effectiveness: Alpha-glucosidase inhibitors can modestly reduce blood glucose levels and help improve glycemic control. They are generally used in conjunction with lifestyle changes and other medications.
Side Effects: Common side effects include gastrointestinal symptoms such as bloating, gas, and diarrhea.
Considerations: Alpha-glucosidase inhibitors are less commonly used as a primary treatment for prediabetes but can be beneficial in specific situations where postprandial glucose control is a significant concern.
GLP-1 Receptor Agonists
Glucagon-like peptide-1 (GLP-1) receptor agonists, such as liraglutide and exenatide, are a class of medications that mimic the action of the GLP-1 hormone. They help regulate blood glucose levels by enhancing insulin secretion, suppressing glucagon release, and slowing gastric emptying.
Mechanism of Action: GLP-1 receptor agonists stimulate insulin secretion in response to meals, inhibit glucagon release, and promote satiety, which can lead to weight loss.
Effectiveness: These medications can improve glycemic control and have been shown to have potential benefits for weight management. They are more commonly used in type 2 diabetes but may be considered for prediabetes in certain cases.
Side Effects: Potential side effects include gastrointestinal issues, such as nausea and vomiting, as well as a risk of pancreatitis. They are also associated with a low risk of hypoglycemia.
Considerations: GLP-1 receptor agonists are typically used for patients who also have obesity or who have not achieved adequate glucose control with other medications.
DPP-4 Inhibitors
Dipeptidyl peptidase-4 (DPP-4) inhibitors, such as sitagliptin, saxagliptin, and linagliptin, are medications that help regulate blood glucose levels by enhancing the body’s own insulin response and decreasing glucose production.
Mechanism of Action: DPP-4 inhibitors work by preventing the breakdown of incretin hormones, which are involved in stimulating insulin secretion and suppressing glucagon release.
Effectiveness: These medications can modestly improve glycemic control and are generally well-tolerated. They are less effective than metformin but may be considered when metformin is not suitable.
Side Effects: Common side effects include respiratory infections, headache, and gastrointestinal issues. There is a potential risk of pancreatitis, although it is rare.
Considerations: DPP-4 inhibitors are usually reserved for patients who cannot tolerate metformin or need additional glycemic control. They are not typically used as first-line therapy for prediabetes.
SGLT2 Inhibitors
Sodium-glucose cotransporter-2 (SGLT2) inhibitors, such as empagliflozin, canagliflozin, and dapagliflozin, are a newer class of medications that work by preventing glucose reabsorption in the kidneys, leading to increased glucose excretion in the urine.
Mechanism of Action: SGLT2 inhibitors block the SGLT2 protein in the kidneys, which is responsible for reabsorbing glucose from urine back into the bloodstream. This results in lower blood glucose levels and a reduction in overall blood glucose levels.
Effectiveness: These medications can effectively lower blood glucose levels and have shown benefits in weight loss and blood pressure reduction. They are more commonly used in type 2 diabetes but may be considered for prediabetes in certain cases.
Side Effects: Common side effects include urinary tract infections, increased urination, and genital yeast infections. There is also a risk of dehydration and electrolyte imbalances.
Considerations: SGLT2 inhibitors are generally used in patients with type 2 diabetes but may be considered for prediabetes when other medications are not effective. They should be used cautiously in patients with renal impairment.
Choosing the Right Medication
The choice of medication for managing prediabetes depends on various factors, including:
Individual Health Profile: Considerations such as kidney function, cardiovascular health, and the presence of other health conditions are important in determining the most appropriate medication.
Side Effect Profile: Each medication has a unique side effect profile, and it is essential to choose a medication that minimizes the risk of adverse effects for the individual patient.
Cost and Accessibility: Medication costs and insurance coverage may impact the choice of therapy. It is important to consider the affordability and availability of medications when making treatment decisions.
Combining Medications
In some cases, a combination of medications may be necessary to achieve optimal glucose control. Combining medications can help address multiple aspects of blood glucose regulation and may be more effective than using a single medication alone. However, careful management is required to avoid potential drug interactions and to monitor for side effects.
Monitoring and Follow-Up
Regular monitoring and follow-up are essential for managing prediabetes effectively. This includes:
Blood Glucose Monitoring: Regular monitoring of blood glucose levels helps assess the effectiveness of treatment and make necessary adjustments.
HbA1c Testing: Periodic HbA1c tests provide a long-term view of blood glucose control and help evaluate the need for medication adjustments.
Lifestyle Assessment: Ongoing evaluation of lifestyle factors, such as diet and physical activity, is important for ensuring that lifestyle modifications are maintained and optimized.
See also: What Are the 5 Major Complications of Diabetes?
Conclusion
Managing prediabetes effectively requires a comprehensive approach that includes lifestyle modifications and, in some cases, medication. Medications such as metformin, TZDs, alpha-glucosidase inhibitors, GLP-1 receptor agonists, DPP-4 inhibitors, and SGLT2 inhibitors can play a valuable role in managing blood glucose levels and preventing the progression to type 2 diabetes. The choice of medication should be individualized based on patient-specific factors and the potential benefits and risks of each treatment. Through careful management and regular monitoring, it is possible to achieve and maintain optimal glucose control and reduce the risk of developing type 2 diabetes.
Related topics:
What Blood Test for Type 2 Diabetes?