Type 1 diabetes is a chronic autoimmune condition in which the body’s immune system attacks and destroys the insulin-producing beta cells in the pancreas. Unlike type 2 diabetes, which often develops due to lifestyle factors and insulin resistance, type 1 diabetes is primarily characterized by the body’s inability to produce insulin. This condition usually develops in children and young adults but can occur at any age.
Diagnosing type 1 diabetes early is crucial to prevent severe complications such as diabetic ketoacidosis (DKA) and to begin appropriate treatment, which typically involves insulin therapy. In this article, we will explore the various tests used to diagnose type 1 diabetes, their significance, and what patients and healthcare providers should consider when interpreting results.
Understanding Type 1 Diabetes and Its Symptoms
Type 1 Diabetes Overview
Type 1 diabetes occurs when the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. Without insulin, the body cannot regulate blood glucose levels, leading to hyperglycemia (high blood sugar). Since type 1 diabetes requires insulin for survival, early and accurate diagnosis is critical for initiating treatment and managing the disease.
Common Symptoms of Type 1 Diabetes
The symptoms of type 1 diabetes can develop rapidly, often over a few weeks or even days. Common symptoms include:
Frequent urination (polyuria): High blood sugar levels cause the kidneys to excrete excess glucose in the urine, leading to increased urination.
Excessive thirst (polydipsia): The increased urination causes dehydration, leading to excessive thirst.
Unexplained weight loss: Despite increased appetite, the body cannot effectively use glucose for energy, resulting in weight loss.
Extreme hunger (polyphagia): The body’s inability to use glucose for energy leads to increased hunger.
Fatigue: Lack of insulin means the body’s cells are deprived of glucose, causing fatigue and weakness.
Blurred vision: High blood sugar can cause swelling in the lens of the eye, leading to blurred vision.
Irritability or mood changes: The effects of high blood sugar can also lead to irritability and mood swings.
These symptoms should prompt immediate medical attention, as they can quickly progress to more severe complications if not treated promptly.
Key Tests for Diagnosing Type 1 Diabetes
Several tests are used to diagnose type 1 diabetes. These tests not only confirm the presence of diabetes but also help distinguish type 1 from type 2 diabetes and other forms of the disease. Here, we will discuss the most commonly used diagnostic tests for type 1 diabetes.
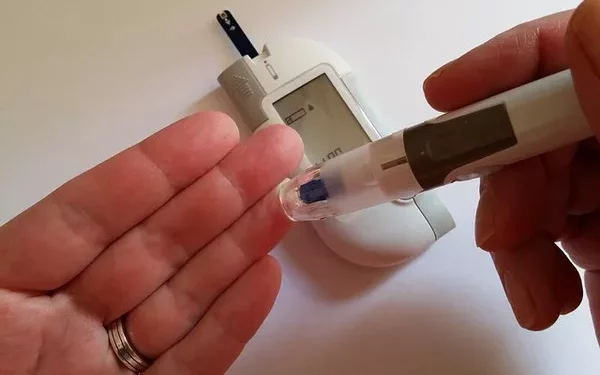
1. Blood Glucose Tests
Blood glucose tests are the most basic and commonly used tests for diagnosing diabetes. These tests measure the level of glucose in the blood and can be performed at any time of the day.
Random Plasma Glucose Test: This test measures blood glucose levels at any time, regardless of when the patient last ate. A random plasma glucose level of 200 mg/dL (11.1 mmol/L) or higher, accompanied by symptoms of diabetes, strongly suggests diabetes.
Fasting Plasma Glucose Test (FPG): This test measures blood glucose after the patient has fasted for at least 8 hours. A fasting plasma glucose level of 126 mg/dL (7.0 mmol/L) or higher on two separate occasions indicates diabetes.
Oral Glucose Tolerance Test (OGTT): The OGTT measures blood glucose before and 2 hours after consuming a glucose-rich drink. A 2-hour blood glucose level of 200 mg/dL (11.1 mmol/L) or higher suggests diabetes.
While these tests are crucial for diagnosing diabetes, they do not distinguish between type 1 and type 2 diabetes. Further testing is required to confirm the type of diabetes.
2. Hemoglobin A1c Test (HbA1c)
The Hemoglobin A1c test measures the average blood glucose levels over the past 2 to 3 months by assessing the percentage of hemoglobin (a protein in red blood cells) that is glycated (coated with sugar).
Diagnosis Criteria: An A1c level of 6.5% or higher on two separate tests indicates diabetes. A lower threshold, typically between 5.7% and 6.4%, suggests prediabetes.
Advantages: The HbA1c test provides a long-term view of blood glucose levels, making it a useful tool for both diagnosing diabetes and monitoring long-term glucose control.
However, like blood glucose tests, the HbA1c test does not differentiate between type 1 and type 2 diabetes. Additional testing is needed to determine the type of diabetes.
3. C-Peptide Test
The C-peptide test measures the level of C-peptide, a byproduct of insulin production, in the blood. Since C-peptide is released in equal amounts to insulin, this test provides an indirect measure of insulin production.
Low C-Peptide Levels: Low or undetectable levels of C-peptide indicate that the pancreas is producing little or no insulin, which is characteristic of type 1 diabetes.
Differentiating Between Type 1 and Type 2 Diabetes: In type 2 diabetes, patients usually have normal or high C-peptide levels, reflecting insulin resistance rather than a lack of insulin production. Therefore, the C-peptide test is valuable in distinguishing between type 1 and type 2 diabetes.
4. Autoantibody Tests
Autoantibody tests are crucial for diagnosing type 1 diabetes, as they detect the presence of antibodies that attack the body’s own insulin-producing cells. Several types of autoantibodies are associated with type 1 diabetes:
Glutamic Acid Decarboxylase Autoantibodies (GADA): GADA are the most common autoantibodies found in people with type 1 diabetes. Their presence indicates an autoimmune response against the insulin-producing beta cells.
Islet Cell Autoantibodies (ICA): ICA are autoantibodies directed against the islet cells of the pancreas, which produce insulin.
Insulin Autoantibodies (IAA): IAA are autoantibodies that target insulin itself. These are more common in young children with type 1 diabetes.
Zinc Transporter 8 Autoantibodies (ZnT8A): ZnT8A are autoantibodies that target the zinc transporter 8 protein, which is involved in insulin storage and release.
Interpretation of Results: The presence of one or more of these autoantibodies strongly suggests type 1 diabetes. A positive result indicates an autoimmune process that is destroying the beta cells, leading to insulin deficiency.
5. Genetic Testing
Genetic testing is not commonly used for diagnosing type 1 diabetes, but it can be helpful in certain situations. Some genes are associated with an increased risk of developing type 1 diabetes, such as HLA-DR and HLA-DQ genes.
Risk Assessment: Genetic testing may be used in research settings or in cases where there is a strong family history of type 1 diabetes. However, having these genetic markers does not guarantee that a person will develop type 1 diabetes, as environmental factors also play a significant role.
6. Ketone Testing
Ketone testing measures the presence of ketones in the blood or urine. Ketones are byproducts of fat breakdown that accumulate when the body cannot use glucose for energy due to a lack of insulin.
Testing for Diabetic Ketoacidosis (DKA): High levels of ketones indicate diabetic ketoacidosis (DKA), a life-threatening complication of type 1 diabetes that requires immediate medical attention.
When to Test: Ketone testing is often used in emergency settings when a person presents with symptoms of DKA, such as nausea, vomiting, abdominal pain, rapid breathing, and confusion.
7. Glucose Tolerance Testing in Pregnancy (Gestational Diabetes)
While type 1 diabetes is not the same as gestational diabetes, which occurs during pregnancy, glucose tolerance testing is sometimes performed on pregnant women to identify undiagnosed type 1 diabetes or to monitor glucose levels in women with a history of type 1 diabetes.
Importance of Testing During Pregnancy: Women with type 1 diabetes require careful monitoring during pregnancy to manage blood glucose levels and reduce the risk of complications for both the mother and baby.
Interpreting Test Results
Understanding the results of these tests is crucial for diagnosing type 1 diabetes and initiating the appropriate treatment. Here are key points to consider:
1. High Blood Glucose Levels
Persistently high blood glucose levels, whether identified through random plasma glucose tests, fasting plasma glucose tests, or HbA1c tests, are indicative of diabetes. However, further testing is needed to confirm whether it is type 1 or type 2 diabetes.
2. Low C-Peptide Levels
Low C-peptide levels suggest that the pancreas is not producing enough insulin, which is characteristic of type 1 diabetes. This test helps distinguish type 1 diabetes from type 2 diabetes, where C-peptide levels are usually normal or elevated.
3. Presence of Autoantibodies
The presence of one or more diabetes-related autoantibodies strongly suggests type 1 diabetes. Autoantibody testing is crucial for confirming the diagnosis and differentiating type 1 diabetes from other forms of diabetes.
4. Ketone Levels
High ketone levels indicate that the body is breaking down fat for energy due to a lack of insulin. This is a sign of diabetic ketoacidosis (DKA), a serious complication of type 1 diabetes that requires immediate treatment.
5. Genetic Markers
While genetic testing is not commonly used for diagnosis, the presence of certain genetic markers can indicate an increased risk of developing type 1 diabetes. However, genetic testing is usually reserved for research or specific clinical situations.
See also: What Are the Causes of Childhood Diabetes?
Conclusion
Diagnosing type 1 diabetes involves a combination of tests that measure blood glucose levels, insulin production, and the presence of autoantibodies. Early diagnosis is crucial for initiating insulin therapy and managing the disease effectively.
Healthcare providers should consider the patient’s symptoms, medical history, and test results when diagnosing type 1 diabetes. Once diagnosed, ongoing monitoring and management are essential to prevent complications and maintain a good quality of life.
Understanding the different tests available for diagnosing type 1 diabetes allows healthcare providers to make informed decisions and provide the best possible care for their patients. By staying vigilant and proactive, we can ensure early detection and effective management of this lifelong condition.
Related topics: