Monitoring blood sugar levels is a critical component of diabetes management, particularly in a hospital setting. For individuals with diabetes or those experiencing blood sugar irregularities, accurate and timely monitoring is essential to prevent complications and ensure optimal care. But how often are blood sugars checked in the hospital? The frequency of blood glucose monitoring depends on various factors, including the patient’s condition, type of diabetes, type of treatment, and overall health status. This article will delve into the intricacies of blood sugar monitoring in hospitals, covering different patient scenarios and the rationale behind specific monitoring protocols.
The Importance of Blood Sugar Monitoring in Hospitals
Hospitalized patients with diabetes or hyperglycemia (high blood sugar) require careful monitoring of their blood glucose levels to manage their condition effectively and prevent complications such as diabetic ketoacidosis, hypoglycemia, or hyperglycemic hyperosmolar syndrome. In non-diabetic patients, acute illness, surgery, infections, or medications such as steroids can induce hyperglycemia, even in those without a history of diabetes. Additionally, hypoglycemia can occur due to fasting, medication errors, or other complications.
Monitoring blood sugar levels in the hospital allows healthcare providers to:
Adjust insulin and other medications: Frequent blood glucose checks help clinicians tailor insulin therapy and oral hypoglycemic agents based on the patient’s changing needs.
Prevent complications: Continuous monitoring can prevent the severe complications of uncontrolled diabetes, such as diabetic ketoacidosis (DKA), hyperosmolar hyperglycemic state (HHS), or severe hypoglycemia.
Ensure safe recovery: In patients recovering from surgery, trauma, or other critical conditions, maintaining stable blood sugar levels supports the healing process and reduces the risk of infection or other complications.
Blood Sugar Monitoring Protocols in Hospitals
The frequency of blood sugar monitoring in hospitals is determined by various protocols, which are often individualized based on the patient’s specific condition and the type of diabetes. In most cases, blood sugar checks occur several times a day, but the exact frequency can vary based on the patient’s needs.
1. Patients with Type 1 Diabetes
Patients with type 1 diabetes, who rely on exogenous insulin, often require intensive blood sugar monitoring. The body of a person with type 1 diabetes does not produce insulin, so careful regulation of insulin therapy is necessary to avoid hypo- or hyperglycemia.
In a hospital setting, blood sugar levels in type 1 diabetics are typically checked:
Before meals: Preprandial blood glucose monitoring is essential to determine the appropriate insulin dose before food intake.
Before bedtime: Checking blood glucose before sleep helps prevent nocturnal hypoglycemia.
Possibly during the night: In some cases, especially in newly diagnosed patients or those with unstable blood sugars, a middle-of-the-night check may be conducted to prevent hypoglycemia.
Before and after physical activity: Physical activity can have significant effects on blood sugar levels, so monitoring before and after exercise may be needed.
During illness or periods of stress: Illness and stress can cause fluctuations in blood sugar levels, so more frequent checks are often necessary during these times.
2. Patients with Type 2 Diabetes
Patients with type 2 diabetes may or may not be insulin-dependent. The frequency of blood sugar checks in hospitalized type 2 diabetics depends on the type of treatment they receive. Patients on insulin therapy generally require more frequent monitoring than those managing their diabetes with oral medications or lifestyle changes.
Blood sugar levels in hospitalized type 2 diabetics are generally checked:
Before meals: This helps determine whether insulin or oral hypoglycemic agents are needed.
Before bedtime: A nighttime check ensures blood glucose levels remain within a safe range overnight.
In response to symptoms: If patients exhibit symptoms of hypoglycemia (shakiness, sweating, confusion) or hyperglycemia (increased thirst, frequent urination), additional blood sugar checks are warranted.
During acute illness or infection: Blood sugar levels tend to rise during periods of acute illness, infection, or surgery, so monitoring is typically more frequent during these times.
After changes in medication: When medications are adjusted, especially insulin, more frequent blood sugar checks help determine the effectiveness of the new regimen.
3. Patients in the Intensive Care Unit (ICU)
For critically ill patients, blood sugar control is a priority regardless of whether they have a history of diabetes. Hyperglycemia in the ICU can result from stress responses, infections, or medications such as corticosteroids. Hypoglycemia, on the other hand, can result from inadequate nutritional support or over-treatment with insulin.
In the ICU, blood sugar monitoring is often more frequent due to the unstable nature of the patients’ conditions. Depending on the patient’s status, blood glucose may be checked:
Every 1-2 hours: For patients receiving intravenous insulin therapy, frequent checks are needed to adjust insulin infusion rates.
Every 4-6 hours: For less critical patients or those receiving subcutaneous insulin, blood sugars may be checked every 4-6 hours.
After significant events: Any changes in a patient’s condition, such as a new infection, surgery, or medication change, may prompt more frequent blood sugar monitoring.
4. Post-Surgical Patients
Surgery can significantly impact blood sugar levels due to the stress response, which increases the production of hormones like cortisol that raise blood sugar levels. Postoperative hyperglycemia is common, even in patients without diabetes, and is associated with an increased risk of infections and other complications.
Post-surgical patients, especially those with diabetes, generally have their blood sugars checked:
Every 4-6 hours: This allows healthcare providers to monitor trends and make necessary adjustments to insulin or other medications.
More frequently in the first 24-48 hours post-surgery: During this critical period, blood sugars may be checked more frequently to catch any early signs of hyperglycemia or hypoglycemia.
5. Patients on Steroid Therapy
Steroids, such as prednisone or dexamethasone, are often used in hospitals to treat a variety of conditions, including autoimmune diseases, allergic reactions, and inflammation. However, steroids can cause significant increases in blood sugar levels, a condition known as steroid-induced hyperglycemia.
Patients receiving steroid therapy typically have their blood sugar checked:
Before meals and at bedtime: Regular monitoring allows for timely adjustments in insulin or other hypoglycemic agents to prevent hyperglycemia.
More frequently during the initiation of steroid therapy: When starting steroid treatment, more frequent checks help assess the impact on blood glucose levels.
6. Pregnant Patients with Gestational Diabetes
Pregnant women with gestational diabetes require careful blood sugar monitoring to protect both their health and the health of their baby. Poorly controlled blood sugar during pregnancy can increase the risk of complications such as preeclampsia, preterm birth, and macrosomia (a large baby).
In the hospital, blood sugar checks for women with gestational diabetes are typically performed:
Before meals: Preprandial monitoring helps guide insulin therapy or other treatments.
After meals: Postprandial blood sugar checks are often conducted 1-2 hours after eating to ensure blood sugar levels remain within target ranges.
Before bedtime: This helps prevent nocturnal hypoglycemia or hyperglycemia.
7. Patients with Diabetic Ketoacidosis (DKA) or Hyperosmolar Hyperglycemic State (HHS)
DKA and HHS are acute complications of diabetes that require intensive monitoring and treatment in the hospital setting. DKA occurs primarily in type 1 diabetes, while HHS is more common in type 2 diabetes. Both conditions involve dangerously high blood sugar levels and require immediate medical attention.
In patients with DKA or HHS, blood sugar levels are typically checked:
Every 1-2 hours initially: During the acute phase of treatment, blood sugars are checked frequently to monitor the response to intravenous insulin and fluid therapy.
Every 4 hours once stabilized: After the patient’s blood sugar begins to normalize, the frequency of checks may be reduced to every 4 hours.
8. Non-Diabetic Patients with Hyperglycemia
Many patients without diabetes develop hyperglycemia during hospitalization due to stress, illness, or medications such as steroids. These patients require monitoring to prevent complications and to determine whether they need temporary insulin therapy.
Non-diabetic patients with hyperglycemia may have their blood sugars checked:
Every 4-6 hours: Regular monitoring helps identify trends and guide treatment.
More frequently during periods of acute stress or medication changes: When the patient’s condition changes or if they are receiving treatments that impact blood sugar, monitoring may become more frequent.
Continuous Glucose Monitoring (CGM) in Hospitals
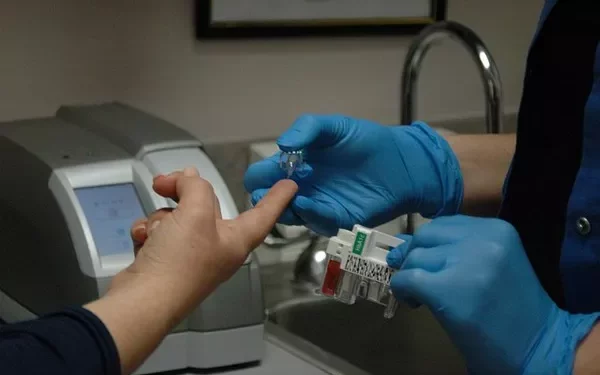
Traditionally, blood glucose monitoring in hospitals is done using fingerstick tests with a glucose meter or laboratory blood tests. However, continuous glucose monitoring (CGM) is becoming more common in the hospital setting. CGM devices provide real-time blood glucose readings and can alert healthcare providers to trends such as rapidly rising or falling blood sugar levels.
CGM can be particularly beneficial for:
ICU patients: Critically ill patients benefit from continuous data that helps prevent both hyperglycemia and hypoglycemia.
Patients with unstable diabetes: Those with frequent fluctuations in blood sugar levels may benefit from the continuous feedback provided by CGM devices.
Postoperative patients: Monitoring blood sugar continuously in the postoperative period can help detect early signs of hyperglycemia or hypoglycemia.
While CGM is not yet standard practice in all hospitals, it is a growing trend that offers more detailed and immediate information about a patient’s blood sugar levels.
Factors Influencing Blood Sugar Monitoring Frequency in Hospitals
Several factors influence how often blood sugars are checked in a hospital setting. These include:
Type of diabetes: Patients with type 1 diabetes or insulin-dependent type 2 diabetes require more frequent monitoring.
Method of treatment: Patients on intravenous insulin or those receiving frequent insulin injections will have their blood sugars checked more often than those on oral medications.
Severity of illness: Critically ill patients, especially those in the ICU, require more intensive monitoring.
Medications: Certain medications, such as steroids or high-dose insulin, necessitate more frequent blood sugar checks.
Presence of complications: Patients with complications such as DKA, HHS, or other acute conditions require frequent monitoring to ensure safe and effective treatment.
See also: What Blood Sugar Level Is Insulin Required
Conclusion
Blood sugar monitoring in hospitals is an essential component of care for patients with diabetes or those experiencing hyperglycemia due to illness, surgery, or medication. The frequency of blood glucose checks varies widely depending on the patient’s condition, treatment regimen, and overall health status. From ICU patients requiring hourly checks to stable post-surgical patients needing monitoring every few hours, the hospital setting demands a tailored approach to blood sugar management. Ensuring that blood sugar levels are consistently monitored and appropriately managed is critical to preventing complications and promoting recovery in hospitalized patients.
Related topics:
Is There a Way to Check Blood Sugar Without Needles?