Insulin resistance is a condition in which the body’s cells become less responsive to the hormone insulin. This hormone is crucial for regulating blood sugar levels by facilitating the uptake of glucose into cells for energy. When cells become resistant to insulin, glucose accumulates in the bloodstream, leading to elevated blood sugar levels. Insulin resistance is a significant risk factor for developing type 2 diabetes, cardiovascular disease, and other metabolic disorders. Early detection and management are crucial in preventing the progression of these conditions.
One of the primary methods for diagnosing insulin resistance is through specific medical tests. These tests help assess how well the body responds to insulin and can provide critical information for the effective management of insulin resistance. In this article, we will explore the various tests used to diagnose insulin resistance, their methodologies, and their clinical significance.
Understanding Insulin Resistance
Insulin resistance occurs when the body’s cells do not respond effectively to insulin, a hormone produced by the pancreas. Insulin helps cells absorb glucose from the bloodstream for energy or storage. When insulin resistance develops, the pancreas compensates by producing more insulin, leading to higher levels of both glucose and insulin in the blood. Over time, this can lead to elevated blood sugar levels and eventually to type 2 diabetes.
Several factors contribute to insulin resistance, including obesity, physical inactivity, genetic predisposition, and hormonal imbalances. Identifying and diagnosing insulin resistance early can help in implementing lifestyle changes and medical interventions to manage or reverse the condition.
Tests for Diagnosing Insulin Resistance
Several tests are used to diagnose insulin resistance. Each test measures different aspects of insulin sensitivity and glucose metabolism. Here, we will discuss the most commonly used tests:
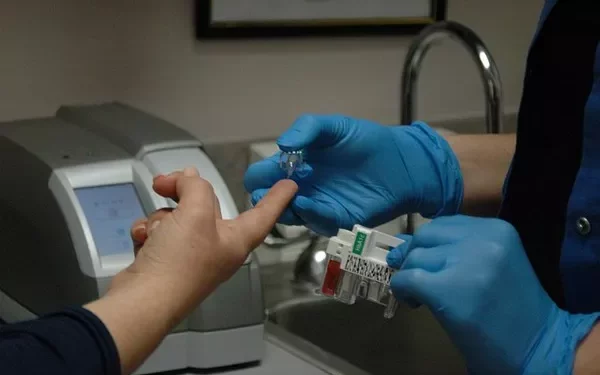
Fasting Blood Glucose Test
The fasting blood glucose test measures blood sugar levels after an overnight fast. While this test alone cannot diagnose insulin resistance, it is often used as a preliminary screening tool. Elevated fasting blood glucose levels can indicate insulin resistance or other metabolic disorders.
Methodology:
- The patient fasts for at least 8 hours before the test.
- A blood sample is taken from the patient’s vein.
- The blood glucose level is measured and compared to normal reference ranges.
Normal Range:
- Fasting blood glucose level < 100 mg/dL (5.6 mmol/L) is considered normal.
- A level between 100 and 125 mg/dL (5.6 to 6.9 mmol/L) is considered prediabetes.
- A level ≥ 126 mg/dL (7.0 mmol/L) on two separate occasions indicates diabetes.
Oral Glucose Tolerance Test (OGTT)
The Oral Glucose Tolerance Test (OGTT) evaluates how the body processes glucose over a specific period. It is more sensitive than the fasting blood glucose test for detecting insulin resistance and glucose intolerance.
Methodology:
- The patient fasts overnight.
- A fasting blood glucose sample is taken.
- The patient then drinks a glucose solution (usually containing 75 grams of glucose).
- Blood samples are taken at intervals (usually at 1 hour and 2 hours) to measure glucose levels.
Normal Range:
- Fasting glucose: < 100 mg/dL (5.6 mmol/L)
- 1-hour glucose: < 180 mg/dL (10.0 mmol/L)
- 2-hour glucose: < 140 mg/dL (7.8 mmol/L)
- Levels above these ranges indicate varying degrees of glucose intolerance or diabetes.
Hemoglobin A1c Test (HbA1c)
The Hemoglobin A1c (HbA1c) test measures the average blood glucose levels over the past 2-3 months. While it is primarily used to diagnose and monitor diabetes, it can also provide insights into insulin resistance.
Methodology:
- A blood sample is taken from the patient’s vein.
- The percentage of hemoglobin molecules that have glucose attached to them (glycated hemoglobin) is measured.
Normal Range:
- HbA1c level < 5.7% is considered normal.
- An HbA1c level between 5.7% and 6.4% indicates prediabetes.
- An HbA1c level ≥ 6.5% indicates diabetes.
Homeostasis Model Assessment of Insulin Resistance (HOMA-IR)
The Homeostasis Model Assessment of Insulin Resistance (HOMA-IR) is a mathematical model used to estimate insulin resistance based on fasting blood glucose and insulin levels. It provides a more direct measure of insulin sensitivity.
Methodology:
- The patient fasts overnight.
- Fasting blood samples are taken to measure both glucose and insulin levels.
Normal Range:
- Values < 1.0 are generally considered to indicate normal insulin sensitivity.
- Values ≥ 1.0 suggest varying degrees of insulin resistance.
Insulin Tolerance Test (ITT)
The Insulin Tolerance Test (ITT) measures how effectively insulin lowers blood glucose levels. This test is less commonly used due to its complexity and potential risks, but it provides valuable information about insulin sensitivity.
Methodology:
- The patient fasts overnight.
- A baseline blood glucose sample is taken.
- Insulin is administered intravenously.
- Blood glucose levels are measured at regular intervals (usually every 15-30 minutes) after insulin administration.
Normal Range:
- The specific response to insulin varies among individuals, but a significant decrease in blood glucose levels indicates normal insulin sensitivity.
Clamp Techniques
The hyperinsulinemic-euglycemic clamp technique is considered the gold standard for measuring insulin sensitivity. It involves maintaining a constant high level of insulin while infusing glucose to keep blood glucose levels stable. This method provides precise measurements of insulin sensitivity but is complex and typically used in research settings.
Methodology:
- The patient fasts overnight.
- Insulin is infused continuously to achieve high levels.
- Glucose is infused to maintain euglycemia (normal blood glucose levels).
- Insulin sensitivity is determined based on the amount of glucose required to maintain normal blood glucose levels.
Normal Range:
- The specific values depend on the glucose infusion rate required to maintain euglycemia.
Interpreting Test Results
Interpreting the results of these tests requires an understanding of the normal ranges and how deviations can indicate insulin resistance. In clinical practice, multiple tests are often used in combination to provide a comprehensive assessment of insulin sensitivity.
Fasting Blood Glucose Test Results:
Elevated fasting blood glucose levels suggest that the body is struggling to regulate blood sugar, which can be indicative of insulin resistance. However, this test alone does not confirm insulin resistance, as other conditions can also cause high blood sugar levels.
Oral Glucose Tolerance Test Results:
Abnormal glucose levels at 1 hour or 2 hours after consuming the glucose solution indicate impaired glucose tolerance or diabetes. The OGTT is particularly useful for diagnosing insulin resistance because it assesses the body’s ability to handle a glucose load over time.
Hemoglobin A1c Test Results:
An elevated HbA1c level suggests that blood glucose levels have been consistently high over the past 2-3 months. This test is useful for monitoring long-term glucose control and can provide insights into the effectiveness of management strategies for insulin resistance.
HOMA-IR Results:
A higher HOMA-IR value indicates greater insulin resistance. This test is valuable for estimating insulin sensitivity and can help in diagnosing insulin resistance before symptoms become apparent.
Insulin Tolerance Test Results:
A significant decrease in blood glucose levels after insulin administration indicates normal insulin sensitivity. Conversely, a minimal change in glucose levels suggests insulin resistance.
Clamp Technique Results:
The clamp technique provides detailed information about insulin sensitivity. A lower glucose infusion rate required to maintain euglycemia indicates higher insulin sensitivity, while a higher rate suggests insulin resistance.
Clinical Significance and Management
Diagnosing insulin resistance is essential for preventing and managing type 2 diabetes and other related conditions. Once diagnosed, insulin resistance can be managed through lifestyle changes, medications, and regular monitoring.
Lifestyle Modifications:
Diet: Adopting a balanced diet with a focus on low-glycemic index foods can help in managing blood sugar levels. Reducing intake of processed foods and sugary beverages is also beneficial.
Exercise: Regular physical activity improves insulin sensitivity and helps in maintaining a healthy weight.
Weight Management: Losing excess weight can significantly improve insulin sensitivity and reduce the risk of developing type 2 diabetes.
Medications:
In some cases, medications such as metformin may be prescribed to help improve insulin sensitivity and manage blood glucose levels.
Monitoring and Follow-up:
Regular monitoring of blood glucose levels and periodic testing for insulin resistance can help in assessing the effectiveness of management strategies and making necessary adjustments.
See also: How To Lose Weight While Insulin Resistance
Conclusion
Insulin resistance is a significant health condition that can lead to type 2 diabetes and other metabolic disorders. Accurate diagnosis is crucial for effective management, and several tests are available to assess insulin sensitivity. These include fasting blood glucose tests, oral glucose tolerance tests, hemoglobin A1c tests, HOMA-IR, insulin tolerance tests, and clamp techniques. Each test provides valuable information about how well the body responds to insulin and helps in identifying insulin resistance early.
Managing insulin resistance involves lifestyle modifications, medications, and regular monitoring to prevent the progression of related conditions. By understanding and utilizing these diagnostic tests, healthcare providers can better manage insulin resistance and improve patient outcomes.
Related topics:
What Does Insulin Resistance Do?