Dizziness is a common symptom that can arise from various underlying conditions, and in the context of diabetes, it can be particularly concerning. Diabetes, especially type 2 diabetes, can lead to a range of complications that affect the body’s ability to maintain balance and regulate blood pressure, contributing to episodes of dizziness. Understanding the connection between dizziness and diabetes, its potential causes, and how to address it is crucial for effective diabetes management and overall health.
Understanding Dizziness
Dizziness is a broad term that can describe a range of sensations, including lightheadedness, vertigo, unsteadiness, and faintness. It can occur suddenly or gradually and may last for a few seconds or persist over a longer period. The sensation of dizziness can be disorienting and may affect daily activities and quality of life.
Types of Dizziness
Lightheadedness: A feeling of faintness or being about to faint. This is often caused by a drop in blood pressure or dehydration.
Vertigo: The sensation that you or your surroundings are spinning. Vertigo is often related to inner ear problems or neurological conditions.
Unsteadiness: A feeling of imbalance or difficulty maintaining coordination. This can be associated with problems in the inner ear or nervous system.
Faintness: A sensation of impending loss of consciousness, often associated with a significant drop in blood pressure.
Dizziness and Type 2 Diabetes
In individuals with type 2 diabetes, dizziness can be attributed to several factors related to the disease and its complications. Understanding these factors is essential for effective management and prevention strategies.
1. Hypoglycemia (Low Blood Sugar)
One of the most common causes of dizziness in diabetes is hypoglycemia, or low blood sugar. When blood glucose levels drop below the normal range, it can lead to symptoms such as dizziness, sweating, shaking, and confusion.
Causes of Hypoglycemia: Hypoglycemia can occur due to several reasons, including excessive insulin or other diabetes medications, skipping meals, increased physical activity, or alcohol consumption.
Symptoms: Symptoms of hypoglycemia include dizziness, sweating, trembling, headache, and irritability. In severe cases, it can lead to loss of consciousness or seizures.
Management: Immediate treatment involves consuming fast-acting carbohydrates, such as glucose tablets, fruit juice, or sugary snacks. It’s important for individuals with diabetes to monitor their blood sugar levels regularly and adjust their medication or meal plans as needed.
2. Hyperglycemia (High Blood Sugar)
Conversely, hyperglycemia, or high blood sugar, can also contribute to dizziness. Elevated blood glucose levels can lead to dehydration and electrolyte imbalances, which can affect blood pressure and cause dizziness.
Causes of Hyperglycemia: Hyperglycemia can result from inadequate insulin or medication, poor dietary choices, stress, or illness.
Symptoms: Along with dizziness, symptoms of hyperglycemia include increased thirst, frequent urination, fatigue, and blurred vision.
Management: Treatment involves monitoring blood glucose levels, adjusting insulin or medication doses, staying hydrated, and following a balanced diet. Severe cases of hyperglycemia may require medical intervention and insulin adjustments.
3. Orthostatic Hypotension
Orthostatic hypotension, or postural hypotension, is a condition characterized by a significant drop in blood pressure when standing up from a sitting or lying position. This can lead to dizziness or lightheadedness.
Causes in Diabetes: Diabetes can affect the autonomic nervous system, leading to impaired regulation of blood pressure. This can be exacerbated by dehydration, medications, or rapid changes in posture.
Symptoms: Symptoms include dizziness, lightheadedness, and faintness when standing up. It may be accompanied by blurred vision or a feeling of weakness.
Management: Management involves rising slowly from sitting or lying positions, staying well-hydrated, and wearing compression stockings if recommended. It’s also important to review medications with a healthcare provider to avoid potential side effects.
4. Diabetic Neuropathy
Diabetic neuropathy is a type of nerve damage that occurs as a complication of diabetes. It can affect various parts of the body, including the autonomic nervous system, which regulates blood pressure and balance.
Symptoms: Diabetic neuropathy can lead to symptoms such as dizziness, unsteadiness, and difficulty maintaining balance. It may also cause numbness, tingling, or pain in the extremities.
Management: Managing diabetic neuropathy involves controlling blood sugar levels, using medications for pain relief, and engaging in physical therapy to improve balance and coordination. Regular monitoring and preventive care are essential for managing this complication.
5. Dehydration
Dehydration can occur in individuals with diabetes due to increased urination from high blood sugar levels. Dehydration can affect blood pressure and contribute to dizziness.
Causes of Dehydration: High blood sugar levels can lead to excessive urination, which depletes the body of fluids and electrolytes.
Symptoms: Symptoms of dehydration include dizziness, dry mouth, reduced urine output, and dark-colored urine.
Management: Staying hydrated by drinking plenty of fluids and managing blood sugar levels effectively can help prevent dehydration. Electrolyte solutions may be recommended in severe cases.
6. Medications
Certain medications used to manage diabetes and its complications can have side effects that include dizziness. This can occur due to the effects of medications on blood pressure, blood sugar levels, or the central nervous system.
Types of Medications: Common medications that may cause dizziness include insulin, oral hypoglycemic agents, and medications for hypertension or cholesterol.
Management: If dizziness is a side effect of medication, it is important to consult with a healthcare provider to review and potentially adjust the medication regimen. Proper dosing and monitoring can help minimize side effects.
7. Cardiovascular Issues
Individuals with diabetes are at an increased risk of cardiovascular problems, including hypertension and heart disease, which can contribute to dizziness.
Causes: Cardiovascular issues can affect blood flow and pressure, leading to dizziness and lightheadedness. Conditions such as atherosclerosis or heart failure may be involved.
Symptoms: Symptoms of cardiovascular issues include dizziness, shortness of breath, chest pain, and palpitations.
Management: Managing cardiovascular health involves controlling blood sugar levels, following a heart-healthy diet, engaging in regular physical activity, and taking medications as prescribed.
8. Hypoglycemia Unawareness
Hypoglycemia unawareness occurs when individuals with diabetes do not experience the typical symptoms of low blood sugar, such as dizziness or sweating. This can make it difficult to recognize and address hypoglycemia promptly.
Causes: This condition may result from long-term diabetes, frequent episodes of hypoglycemia, or autonomic neuropathy.
Symptoms: Individuals may experience more severe symptoms of hypoglycemia without the usual warning signs, including dizziness, confusion, or loss of consciousness.
Management: Regular blood sugar monitoring and adjustments in diabetes management can help prevent hypoglycemia unawareness. Educating individuals about recognizing and managing hypoglycemia is crucial.
Preventive Measures and Management Strategies
To effectively manage dizziness related to diabetes, it is important to adopt a comprehensive approach that includes:
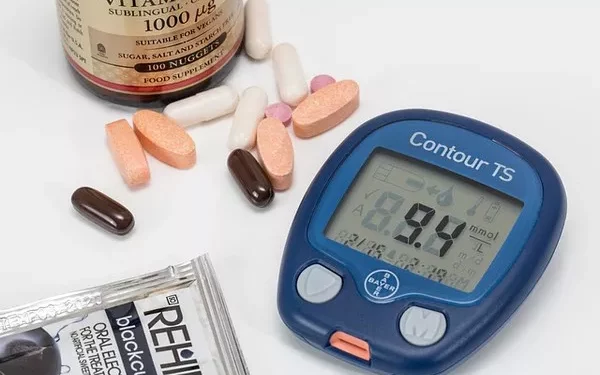
Regular Monitoring: Frequent monitoring of blood glucose levels helps in detecting and managing fluctuations that could lead to dizziness. Continuous glucose monitoring systems can provide real-time data and trends.
Medication Management: Review and adjust medications with a healthcare provider to minimize side effects and optimize treatment. It’s essential to follow prescribed dosages and schedules.
Hydration: Maintain adequate hydration by drinking plenty of water and monitoring for signs of dehydration. Address high blood sugar levels to prevent excessive urination.
Diet and Exercise: Follow a balanced diet that helps in maintaining stable blood sugar levels. Engage in regular physical activity to support cardiovascular health and improve overall well-being.
Lifestyle Adjustments: Make gradual changes in posture to avoid orthostatic hypotension, manage stress, and ensure proper rest and recovery.
Medical Evaluation: Regular check-ups with healthcare providers to assess for complications such as diabetic neuropathy, cardiovascular issues, and medication side effects are essential for comprehensive care.
See also: What is Type 11 Diabetes?
Conclusion
Dizziness can be a significant symptom for individuals with type 2 diabetes, arising from various underlying causes related to the disease and its complications. Hypoglycemia, hyperglycemia, orthostatic hypotension, diabetic neuropathy, dehydration, medication side effects, cardiovascular issues, and hypoglycemia unawareness can all contribute to dizziness. Understanding these connections and implementing effective management strategies are crucial for maintaining optimal health and quality of life. Regular monitoring, medication management, proper hydration, a balanced diet, and lifestyle adjustments play key roles in addressing dizziness and preventing its impact on daily activities. As always, working closely with healthcare providers and staying informed about diabetes management can help in achieving better outcomes and enhancing overall well-being.
Related topics:
What Are SGLT2 Diabetes Drugs?