Monitoring blood sugar levels is a crucial aspect of managing diabetes and maintaining overall health. Blood sugar, or glucose, is the primary source of energy for the body’s cells, and maintaining its levels within a normal range is vital for preventing both short-term and long-term complications. This article delves into the concept of normal sugar range, exploring the factors influencing these levels, methods of measurement, and the implications of deviations from the norm. We will also discuss the importance of personalized targets and provide practical advice for maintaining healthy blood sugar levels.
Understanding Blood Sugar Levels
What is Blood Sugar?
Blood sugar, or glucose, is a type of sugar that circulates in the bloodstream, supplying energy to the body’s cells. It is derived from the carbohydrates we consume and is regulated by insulin, a hormone produced by the pancreas. Insulin facilitates the uptake of glucose into cells, where it can be used for energy production or stored for later use.
Normal Blood Sugar Levels
Normal blood sugar levels vary depending on the time of day and whether the individual has eaten. The following are the typical ranges for fasting blood sugar (measured after at least eight hours without food) and postprandial blood sugar (measured two hours after eating):
Fasting Blood Sugar:
Normal: 70-99 mg/dL (3.9-5.5 mmol/L)
Prediabetes: 100-125 mg/dL (5.6-6.9 mmol/L)
Diabetes: 126 mg/dL (7.0 mmol/L) or higher
Postprandial Blood Sugar:
Normal: Less than 140 mg/dL (7.8 mmol/L)
Prediabetes: 140-199 mg/dL (7.8-11.0 mmol/L)
Diabetes: 200 mg/dL (11.1 mmol/L) or higher
It is essential to note that these values can vary slightly depending on the guidelines used and the individual’s specific circumstances, such as age, overall health, and the presence of other medical conditions.
Hemoglobin A1c (HbA1c)
Hemoglobin A1c (HbA1c) is a blood test that provides an average of blood sugar levels over the past two to three months. It reflects the percentage of glucose attached to hemoglobin, a protein in red blood cells. The HbA1c test is an essential tool for diagnosing diabetes and monitoring long-term glucose control. The target HbA1c levels are as follows:
- Normal: Below 5.7%
- Prediabetes: 5.7%-6.4%
- Diabetes: 6.5% or higher
Factors Influencing Blood Sugar Levels
Blood sugar levels can fluctuate due to various factors. Understanding these factors is crucial for managing diabetes and maintaining healthy glucose levels.
1. Diet
The type and amount of food consumed significantly impact blood sugar levels. Carbohydrates, especially simple sugars, are quickly broken down into glucose, leading to a rapid rise in blood sugar. On the other hand, complex carbohydrates, proteins, and fats cause a slower and more gradual increase. The glycemic index (GI) is a measure that ranks foods based on how quickly they raise blood sugar levels. Low-GI foods are preferable for maintaining stable blood sugar levels.
2. Physical Activity
Exercise has a profound effect on blood sugar levels. Physical activity increases insulin sensitivity, allowing cells to use glucose more effectively. As a result, regular exercise can help lower blood sugar levels and improve overall glucose control. However, intense or prolonged exercise can sometimes lead to hypoglycemia (low blood sugar), especially in individuals taking insulin or certain oral medications.
3. Medications
Various medications, particularly those used to manage diabetes, can affect blood sugar levels. Insulin and certain oral medications, such as sulfonylureas, can lower blood sugar levels. Conversely, some medications, including corticosteroids and certain psychiatric drugs, can raise blood sugar levels. It is crucial for individuals with diabetes to work closely with their healthcare providers to adjust medications as needed.
4. Stress and Illness
Stress and illness can trigger the release of stress hormones, such as cortisol and adrenaline, which can raise blood sugar levels. Infections, injuries, and other medical conditions can also affect glucose metabolism. Monitoring blood sugar levels during periods of stress or illness is essential to prevent hyperglycemia (high blood sugar) or hypoglycemia.
5. Hormonal Changes
Hormonal fluctuations, such as those occurring during menstruation, pregnancy, or menopause, can impact blood sugar levels. For example, the hormonal changes during pregnancy can lead to gestational diabetes, a condition characterized by elevated blood sugar levels during pregnancy.
Methods of Blood Sugar Measurement
Accurate measurement of blood sugar levels is essential for diagnosing and managing diabetes. Several methods are available for monitoring blood sugar, each with its advantages and limitations.
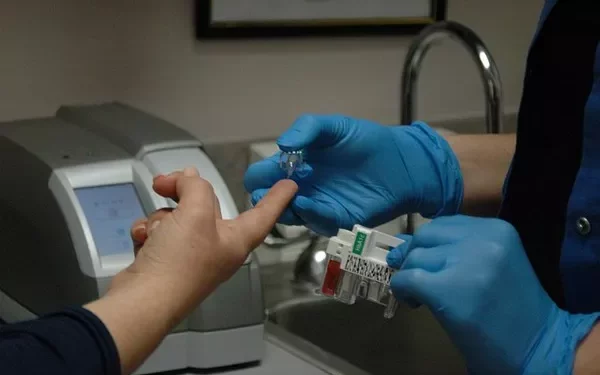
1. Self-Monitoring of Blood Glucose (SMBG)
SMBG involves using a glucose meter and test strips to measure blood sugar levels. It is a convenient and widely used method that allows individuals to check their blood sugar levels at home. SMBG provides real-time information, enabling people to make immediate adjustments to their diet, exercise, or medication.
2. Continuous Glucose Monitoring (CGM)
CGM systems consist of a small sensor inserted under the skin to measure glucose levels in the interstitial fluid. The sensor transmits data to a receiver or smartphone, providing continuous information about glucose levels throughout the day and night. CGM can help identify patterns and trends in blood sugar levels, allowing for better diabetes management.
3. HbA1c Testing
As mentioned earlier, HbA1c testing provides an average of blood sugar levels over the past two to three months. It is a valuable tool for assessing long-term glucose control and is typically measured during routine medical visits.
Implications of Deviations from Normal Blood Sugar Levels
Maintaining blood sugar levels within the normal range is crucial for preventing both acute and chronic complications associated with diabetes.
1. Hyperglycemia (High Blood Sugar)
Hyperglycemia occurs when blood sugar levels are consistently elevated. It can result from insufficient insulin production, insulin resistance, excessive carbohydrate intake, stress, illness, or certain medications. Symptoms of hyperglycemia may include increased thirst, frequent urination, fatigue, blurred vision, and slow-healing wounds.
Prolonged hyperglycemia can lead to serious complications, including:
Diabetic Ketoacidosis (DKA): A potentially life-threatening condition characterized by the buildup of ketones (toxic acids) in the blood, leading to nausea, vomiting, abdominal pain, and confusion.
Hyperosmolar Hyperglycemic State (HHS): A severe condition often seen in individuals with type 2 diabetes, characterized by extreme hyperglycemia and dehydration, leading to altered consciousness and, in severe cases, coma.
Chronic Complications: Long-term hyperglycemia can damage blood vessels, nerves, and organs, increasing the risk of cardiovascular disease, kidney disease, neuropathy, and retinopathy.
2. Hypoglycemia (Low Blood Sugar)
Hypoglycemia occurs when blood sugar levels drop below the normal range. It can result from excessive insulin or medication, insufficient food intake, prolonged exercise, or alcohol consumption. Symptoms of hypoglycemia may include shakiness, sweating, confusion, irritability, dizziness, and, in severe cases, loss of consciousness or seizures.
Prompt treatment of hypoglycemia is crucial to prevent severe complications. Consuming fast-acting carbohydrates, such as glucose tablets or juice, can quickly raise blood sugar levels.
Personalized Blood Sugar Targets
Blood sugar targets can vary based on individual factors such as age, duration of diabetes, comorbidities, and personal preferences. Therefore, it is essential for individuals with diabetes to work closely with their healthcare providers to determine personalized blood sugar targets that balance optimal glucose control with safety and quality of life.
1. Tight Glycemic Control
Tight glycemic control involves maintaining blood sugar levels as close to the normal range as possible. While it can reduce the risk of diabetes-related complications, it also increases the risk of hypoglycemia. Tight glycemic control may be more suitable for younger individuals with a shorter duration of diabetes and a lower risk of hypoglycemia.
2. Less Stringent Glycemic Control
Less stringent glycemic control may be appropriate for older adults, individuals with a longer duration of diabetes, or those at higher risk of hypoglycemia. It involves higher blood sugar targets to reduce the risk of severe hypoglycemia while still aiming for good glucose control.
Tips for Maintaining Healthy Blood Sugar Levels
Maintaining healthy blood sugar levels requires a comprehensive approach that includes lifestyle modifications, medication management, and regular monitoring. Here are some practical tips to help achieve optimal glucose control:
1. Balanced Diet
A balanced diet rich in whole grains, lean proteins, healthy fats, and a variety of fruits and vegetables can help maintain stable blood sugar levels. It is essential to monitor carbohydrate intake, choose low-GI foods, and avoid sugary snacks and beverages.
2. Regular Physical Activity
Engaging in regular physical activity, such as walking, swimming, cycling, or strength training, can improve insulin sensitivity and help regulate blood sugar levels. It is essential to consult with a healthcare provider before starting any new exercise regimen, especially for individuals with diabetes.
3. Medication Adherence
Taking prescribed medications as directed by a healthcare provider is crucial for managing blood sugar levels. This includes insulin, oral medications, or other treatments. It is essential to communicate with a healthcare provider about any side effects or concerns related to medications.
4. Stress Management
Stress can negatively impact blood sugar levels. Practicing stress-reducing techniques such as meditation, deep breathing exercises, yoga, or spending time in nature can help manage stress and promote overall well-being.
5. Regular Monitoring
Regular monitoring of blood sugar levels, whether through SMBG, CGM, or routine HbA1c testing, is vital for tracking progress and making necessary adjustments to the treatment plan. It also helps in identifying patterns and trends that can inform lifestyle and medication adjustments.
6. Healthy Sleep Habits
Adequate sleep is essential for overall health and blood sugar regulation. Poor sleep can disrupt insulin sensitivity and increase the risk of hyperglycemia. Aim for 7-9 hours of quality sleep per night and establish a consistent sleep routine.
7. Education and Support
Continuous education about diabetes management, including nutrition, exercise, medication, and blood sugar monitoring, empowers individuals to take control of their health. Support from healthcare providers, diabetes educators, and support groups can also provide valuable guidance and motivation.
See also: What’s the Importance of Managing Blood Sugar Levels
Conclusion
Maintaining blood sugar levels within the normal range is a cornerstone of diabetes management and overall health. Understanding the factors that influence blood sugar levels, the methods of measurement, and the implications of deviations from the norm is crucial for preventing complications and achieving optimal glucose control. With personalized targets, lifestyle modifications, and regular monitoring, individuals with diabetes can effectively manage their condition and lead healthy, fulfilling lives. Always consult with healthcare providers to develop a comprehensive and individualized diabetes management plan.
Related topics:
How Long Does It Take to Reverse Prediabetes with Diet?