Hypoglycemia, a condition characterized by abnormally low blood glucose levels, can have significant impacts on the brain, leading to altered mental status. This article delves into the mechanisms by which hypoglycemia affects brain function, the clinical manifestations of hypoglycemia-induced cognitive impairment, and the importance of timely recognition and management in diabetic patients.
The Importance of Glucose for Brain Function
Glucose as the Primary Energy Source
The brain relies almost exclusively on glucose for its energy needs. Neurons, the primary cells of the brain, have a high metabolic rate and require a constant supply of glucose to function optimally. Unlike other tissues, the brain cannot store glucose in significant amounts and is dependent on a continuous supply from the bloodstream.
Glucose Transport to the Brain
Glucose crosses the blood-brain barrier through specialized glucose transporter proteins, primarily GLUT1. These transporters ensure a steady flow of glucose from the blood to the brain, maintaining normal neuronal function and cognitive processes.
Pathophysiology of Hypoglycemia-Induced Altered Mental Status
Mechanisms of Neuronal Dysfunction
Energy Deprivation
When blood glucose levels fall below normal, the brain’s energy supply is compromised. Neurons cannot generate sufficient ATP (adenosine triphosphate), which is essential for maintaining cellular functions, including ion gradients, neurotransmitter release, and synaptic activity. This energy deprivation leads to impaired neuronal function and altered mental status.
Neurotransmitter Imbalance
Hypoglycemia disrupts the balance of neurotransmitters in the brain. Neurotransmitters such as glutamate, gamma-aminobutyric acid (GABA), and acetylcholine are critical for cognitive processes and mood regulation. Hypoglycemia-induced energy deficits can impair the synthesis, release, and reuptake of these neurotransmitters, leading to cognitive and behavioral changes.
Acute Effects of Hypoglycemia on the Brain
Cerebral Blood Flow
Hypoglycemia can lead to changes in cerebral blood flow. As glucose levels drop, the brain responds by increasing blood flow to maintain glucose delivery. However, this compensatory mechanism may be insufficient in severe hypoglycemia, exacerbating neuronal energy deficits and cognitive impairment.
Brain Metabolism
During hypoglycemia, the brain attempts to use alternative energy sources, such as lactate and ketone bodies. However, these substrates are less efficient than glucose and cannot fully compensate for the energy shortfall, resulting in continued neuronal dysfunction.
Clinical Manifestations of Hypoglycemia-Induced Altered Mental Status
Cognitive Symptoms
Confusion
Confusion is a common symptom of hypoglycemia and can range from mild disorientation to profound cognitive impairment. Patients may have difficulty concentrating, remembering information, and processing thoughts.
Memory Impairment
Hypoglycemia can cause both short-term and long-term memory deficits. Patients may struggle to recall recent events or learn new information, impacting their ability to perform daily activities.
Impaired Judgment
Hypoglycemia can impair judgment and decision-making abilities. Patients may make poor or irrational decisions, increasing the risk of accidents and injuries.
Behavioral Symptoms
Agitation and Irritability
Low blood glucose levels can lead to mood changes, including agitation and irritability. Patients may become easily frustrated or anxious, which can further complicate their cognitive impairment.
Aggression
In some cases, hypoglycemia can trigger aggressive behavior. This aggression may be verbal or physical, posing challenges for caregivers and healthcare providers.
Neurological Symptoms
Seizures
Severe hypoglycemia can provoke seizures due to the profound disruption of neuronal function. These seizures may be focal or generalized and require immediate medical attention.
Coma
Prolonged or severe hypoglycemia can lead to a hypoglycemic coma, a life-threatening condition characterized by profound unconsciousness. Rapid intervention is crucial to prevent permanent brain damage or death.
Factors Contributing to Hypoglycemia in Diabetes
Insulin Therapy
Overdosing
Insulin therapy is a cornerstone of diabetes management, but improper dosing can lead to hypoglycemia. Overdosing insulin, either by mistake or due to incorrect adjustments, increases the risk of blood glucose dropping too low.
Timing Issues
The timing of insulin administration relative to meals and physical activity is critical. Administering insulin without adequate food intake or during periods of increased physical activity can lead to hypoglycemia.
Oral Hypoglycemic Agents
Certain oral medications used to manage diabetes, such as sulfonylureas and meglitinides, stimulate insulin release from the pancreas. These medications can cause hypoglycemia, particularly if not balanced with food intake.
Lifestyle Factors
Skipped Meals
Skipping meals or not consuming enough carbohydrates can lead to hypoglycemia, especially in patients on insulin or other hypoglycemic agents. Maintaining regular meal patterns is essential for preventing low blood sugar.
Excessive Exercise
Physical activity increases glucose uptake by muscles, which can lower blood glucose levels. Without appropriate adjustments in medication or carbohydrate intake, exercise can precipitate hypoglycemia.
Diagnosing Hypoglycemia
Blood Glucose Measurement
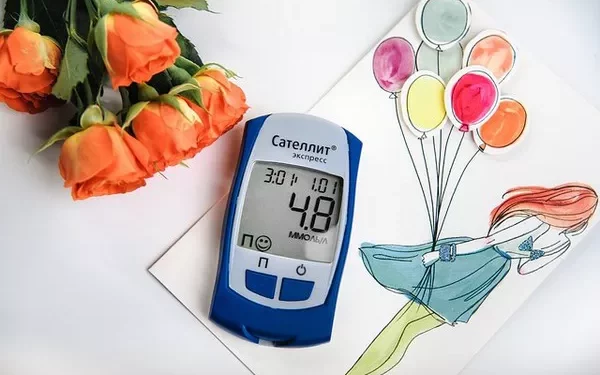
Self-Monitoring
Patients with diabetes should regularly monitor their blood glucose levels using glucometers. Recognizing patterns of low blood glucose can help in adjusting treatment and preventing hypoglycemia.
Continuous Glucose Monitoring (CGM)
CGM devices provide real-time glucose readings, allowing for the detection of hypoglycemia before symptoms become severe. CGM can be particularly useful for patients with frequent hypoglycemia or hypoglycemia unawareness.
Clinical Assessment
Symptoms Evaluation
Healthcare providers should assess patients for symptoms of hypoglycemia, including cognitive and behavioral changes. A thorough history and physical examination can help identify underlying causes and guide treatment.
Laboratory Tests
In some cases, laboratory tests may be necessary to confirm hypoglycemia and investigate potential causes. These tests may include fasting blood glucose, insulin levels, and other metabolic markers.
Management of Hypoglycemia
Immediate Treatment
Rapid Acting Carbohydrates
The first step in treating hypoglycemia is the administration of rapid-acting carbohydrates, such as glucose tablets, fruit juice, or candy. These should be readily available to patients at risk of hypoglycemia.
Glucagon Administration
For severe hypoglycemia, glucagon injection may be necessary. Glucagon stimulates the liver to release stored glucose, rapidly increasing blood glucose levels.
Preventive Strategies
Medication Adjustment
Adjusting the dose and timing of insulin or oral hypoglycemic agents can help prevent hypoglycemia. Patients should work closely with their healthcare providers to tailor their treatment plans based on their individual needs.
Meal Planning
Consistent meal patterns and adequate carbohydrate intake are crucial for preventing hypoglycemia. Patients should be educated on how to balance their diet with their medication regimen.
Physical Activity Management
Patients should be advised on how to adjust their medication and food intake around physical activity. Monitoring blood glucose before, during, and after exercise can help prevent hypoglycemia.
Education and Support
Patient Education
Educating patients on the signs and symptoms of hypoglycemia, proper glucose monitoring, and management strategies is essential. Empowering patients with knowledge can improve their ability to prevent and treat hypoglycemia.
Support Systems
Support from healthcare providers, diabetes educators, and support groups can help patients manage their condition more effectively. Regular follow-ups and personalized care plans can enhance patient outcomes.
Long-Term Implications of Hypoglycemia
Cognitive Function
Recurrent Hypoglycemia
Frequent episodes of hypoglycemia can have long-term effects on cognitive function. Studies suggest that recurrent hypoglycemia may increase the risk of cognitive decline and dementia.
Hypoglycemia Unawareness
Patients with recurrent hypoglycemia may develop hypoglycemia unawareness, where they no longer recognize the early symptoms of low blood glucose. This condition increases the risk of severe hypoglycemia and associated complications.
Quality of Life
Psychological Impact
Hypoglycemia can significantly impact a patient’s quality of life. Fear of hypoglycemia may lead to anxiety, depression, and reduced participation in daily activities.
Social and Occupational Consequences
Altered mental status due to hypoglycemia can affect social interactions and job performance. Patients may struggle with maintaining relationships and fulfilling work responsibilities.
See also: What Medication Do You Take for Hypoglycemia?
Conclusion
Hypoglycemia can cause altered mental status through a complex interplay of neuronal energy deficits, neurotransmitter imbalances, and cerebral blood flow changes. Recognizing the symptoms and understanding the underlying mechanisms are crucial for timely intervention and prevention. As a diabetes doctor, it is essential to educate patients, adjust treatment plans, and provide ongoing support to manage and prevent hypoglycemia effectively. By doing so, we can help patients maintain better cognitive function and overall quality of life.
Related topics:
Type 1 VS Type 2 Hypoglycemia : What’s the Difference