Hyperglycemia, a condition characterized by elevated levels of glucose in the blood, is a hallmark of diabetes. It occurs when the body either doesn’t produce enough insulin or can’t effectively use the insulin it produces. While transient increases in blood sugar levels are not uncommon and can happen due to various factors such as stress, illness, or dietary intake, persistent hyperglycemia can lead to serious health complications. This article delves into why hyperglycemia is bad, exploring its causes, symptoms, short-term and long-term complications, and management strategies.
Causes of Hyperglycemia
Hyperglycemia can result from a variety of factors, both related to lifestyle and underlying medical conditions. Understanding these causes is crucial for effective management and prevention.
Insufficient Insulin Production
Insulin is a hormone produced by the pancreas that regulates blood glucose levels by facilitating the uptake of glucose into cells for energy production. In individuals with type 1 diabetes, the immune system attacks and destroys insulin-producing beta cells in the pancreas, leading to insufficient insulin production and hyperglycemia.
Insulin Resistance
In type 2 diabetes, the body’s cells become resistant to the effects of insulin. This means that even though insulin is present, it is not used effectively, leading to elevated blood sugar levels. Insulin resistance is often associated with obesity, physical inactivity, and genetic predisposition.
Dietary Factors
High carbohydrate intake, especially from simple sugars, can cause spikes in blood glucose levels. Inadequate meal planning or consuming foods with a high glycemic index can lead to hyperglycemia, particularly in individuals with diabetes who require careful management of their diet.
Physical Inactivity
Regular physical activity helps maintain healthy blood glucose levels by increasing insulin sensitivity and facilitating glucose uptake by muscles. Sedentary lifestyles contribute to insulin resistance and poor glycemic control.
Stress and Illness
Stress and illness trigger the release of hormones such as cortisol and adrenaline, which can raise blood glucose levels. Infections, surgeries, and other physical stressors can exacerbate hyperglycemia, making it important to monitor blood sugar closely during such times.
Medications
Certain medications, including corticosteroids, beta-blockers, and some antipsychotics, can interfere with insulin function or increase glucose production, leading to hyperglycemia.
Symptoms of Hyperglycemia
Recognizing the symptoms of hyperglycemia is vital for timely intervention and prevention of complications. Symptoms can vary in severity and may develop gradually.
Common Symptoms
Increased Thirst and Urination: Excess glucose in the blood leads to osmotic diuresis, causing the kidneys to excrete more water and leading to dehydration.
Fatigue: High blood sugar levels can impair the body’s ability to use glucose for energy, resulting in fatigue and weakness.
Blurred Vision: Elevated glucose levels can cause swelling in the lens of the eye, leading to blurred vision.
Headaches: Persistent hyperglycemia can cause headaches due to dehydration and changes in blood flow.
Dry Mouth and Skin: Dehydration from frequent urination can cause dry mouth and skin.
Severe Symptoms
Ketoacidosis: In type 1 diabetes, lack of insulin can lead to the breakdown of fat for energy, producing ketones that can accumulate and lead to diabetic ketoacidosis (DKA), a potentially life-threatening condition characterized by nausea, vomiting, abdominal pain, and confusion.
Hyperosmolar Hyperglycemic State (HHS): In type 2 diabetes, severe hyperglycemia without ketone production can lead to HHS, marked by extreme dehydration, confusion, and coma.
Short-term Complications
Short-term complications of hyperglycemia require immediate attention to prevent further health issues.
Dehydration
Hyperglycemia causes the kidneys to excrete excess glucose through urine, leading to increased water loss and dehydration. Severe dehydration can result in electrolyte imbalances and reduced blood volume, affecting overall health.
Diabetic Ketoacidosis (DKA)
DKA is a serious condition predominantly seen in type 1 diabetes but can occur in type 2 diabetes under certain circumstances. It results from the body’s inability to use glucose for energy, leading to the breakdown of fat and production of ketones. Symptoms include nausea, vomiting, abdominal pain, fruity-smelling breath, and confusion. DKA requires immediate medical intervention.
Infections
High blood sugar levels can impair immune function, making individuals more susceptible to infections. Common infections include urinary tract infections, skin infections, and yeast infections.
Long-term Complications
Chronic hyperglycemia can lead to a range of long-term complications that significantly impact quality of life and increase the risk of mortality.
Cardiovascular Disease
Persistent hyperglycemia contributes to the development of atherosclerosis, a condition characterized by the buildup of plaque in the arteries. This increases the risk of coronary artery disease, heart attacks, and strokes. Individuals with diabetes are at a higher risk of cardiovascular complications due to hyperglycemia-induced damage to blood vessels and nerves.
Neuropathy
High blood sugar levels can damage the nerves, leading to diabetic neuropathy. Symptoms include numbness, tingling, and pain, particularly in the hands and feet. Severe neuropathy can result in loss of sensation, increasing the risk of injuries and infections.
Nephropathy
Hyperglycemia can damage the kidneys’ filtering units, leading to diabetic nephropathy. This condition can progress to chronic kidney disease and ultimately kidney failure, requiring dialysis or a kidney transplant.
Retinopathy
Diabetic retinopathy is a condition where high blood sugar levels damage the blood vessels in the retina, leading to vision problems and potentially blindness. Regular eye exams and good glycemic control are essential to prevent or slow the progression of retinopathy.
Foot Complications
Neuropathy and poor circulation due to hyperglycemia can result in foot ulcers and infections. Severe cases may lead to gangrene and necessitate amputation.
Cognitive Decline
Chronic hyperglycemia has been linked to cognitive decline and an increased risk of developing Alzheimer’s disease. The exact mechanisms are not fully understood, but high blood sugar levels can cause inflammation and oxidative stress, contributing to brain damage.
Management of Hyperglycemia
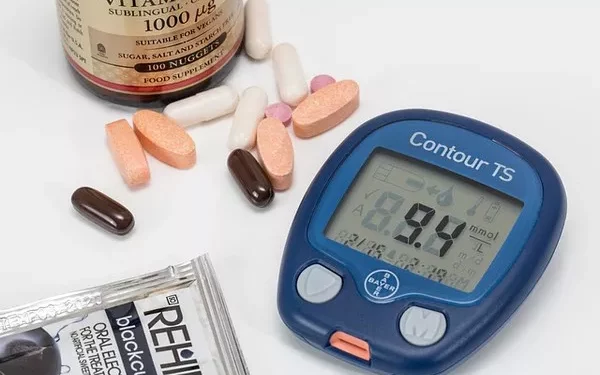
Effective management of hyperglycemia involves a combination of lifestyle modifications, medication, and regular monitoring of blood glucose levels. Here are some key strategies:
Dietary Management
Balanced Diet: A balanced diet with controlled carbohydrate intake is crucial for managing blood sugar levels. Emphasize whole grains, lean proteins, healthy fats, and plenty of vegetables.
Glycemic Index: Choose foods with a low glycemic index, as they have a slower impact on blood glucose levels.
Portion Control: Monitor portion sizes to avoid overeating and to manage blood sugar effectively.
Regular Meals: Eating regular, balanced meals can help maintain stable blood glucose levels.
Physical Activity
Regular Exercise: Engage in regular physical activity, such as walking, cycling, or swimming, to improve insulin sensitivity and promote glucose uptake by muscles.
Strength Training: Incorporate strength training exercises to build muscle mass, which helps improve glucose metabolism.
Medication
Insulin Therapy: For individuals with type 1 diabetes and some with type 2 diabetes, insulin therapy is essential to regulate blood glucose levels.
Oral Medications: Various oral medications can help manage blood sugar levels in type 2 diabetes by increasing insulin production, reducing glucose absorption, or improving insulin sensitivity.
Injectable Medications: In addition to insulin, other injectable medications, such as GLP-1 receptor agonists, can help control blood sugar levels.
Monitoring
Regular Monitoring: Frequent monitoring of blood glucose levels helps track the effectiveness of management strategies and make necessary adjustments.
Continuous Glucose Monitors (CGMs): CGMs provide real-time data on blood glucose levels, allowing for more precise and timely interventions.
Stress Management
Relaxation Techniques: Practice relaxation techniques such as deep breathing, meditation, and yoga to manage stress, which can impact blood sugar levels.
Adequate Sleep: Ensure adequate and quality sleep to support overall health and glycemic control.
Education and Support
Diabetes Education: Participate in diabetes education programs to gain a better understanding of the condition and effective management strategies.
Support Groups: Join support groups for individuals with diabetes to share experiences and receive emotional support.
See also: How Hyperglycemia Causes Hypovolemic Shock
Conclusion
Hyperglycemia is a significant health concern that requires diligent management to prevent both short-term and long-term complications. Understanding the causes, symptoms, and potential consequences of high blood sugar levels is crucial for effective prevention and treatment. By adopting a comprehensive approach that includes dietary management, regular physical activity, medication, and stress management, individuals with hyperglycemia can achieve better glycemic control and improve their overall health and quality of life. Regular monitoring and ongoing education are key components in the successful management of hyperglycemia, enabling individuals to lead healthier, more fulfilling lives.
Related topics:
What Does Hyperglycemia Cause?