Hyperglycemia, commonly known as high blood sugar, is a condition that occurs when the level of glucose in the blood is elevated beyond the normal range. It is a hallmark of diabetes, particularly type 2 diabetes. Understanding the connection between hyperglycemia and type 2 diabetes is crucial for effective management and prevention of complications. This article explores the relationship between hyperglycemia and type 2 diabetes, including causes, symptoms, and strategies for management and prevention.
Understanding Hyperglycemia
Hyperglycemia occurs when there is too much glucose in the blood. Glucose is a vital source of energy for the body’s cells, but high levels can be detrimental. The pancreas produces insulin, a hormone that helps cells absorb glucose from the bloodstream. In hyperglycemia, either the body doesn’t produce enough insulin, or the cells become resistant to insulin’s effects, leading to elevated blood sugar levels.
Causes of Hyperglycemia
Several factors can cause hyperglycemia, including:
- Insufficient Insulin Production: In type 2 diabetes, the pancreas may not produce enough insulin to meet the body’s needs.
- Insulin Resistance: Cells in the body become resistant to the effects of insulin, requiring higher levels of insulin to maintain normal blood sugar levels.
- Dietary Factors: Consuming high amounts of carbohydrates, sugars, and unhealthy fats can cause blood sugar levels to spike.
- Physical Inactivity: Lack of physical activity can reduce the efficiency of glucose uptake by muscles, leading to higher blood sugar levels.
- Stress: Physical or emotional stress can increase the release of stress hormones like cortisol and adrenaline, which can raise blood sugar levels.
- Medications: Certain medications, such as corticosteroids, can increase blood sugar levels.
- Illness or Infection: Illnesses or infections can cause blood sugar levels to rise due to the body’s stress response.
Symptoms of Hyperglycemia
The symptoms of hyperglycemia can vary, but common signs include:
- Increased thirst
- Frequent urination
- Fatigue
- Blurred vision
- Headaches
- Difficulty concentrating
- Unexplained weight loss
- Slow-healing sores or cuts
If left untreated, hyperglycemia can lead to serious complications, such as diabetic ketoacidosis (DKA) in type 1 diabetes and hyperosmolar hyperglycemic state (HHS) in type 2 diabetes.
Understanding Type 2 Diabetes
Type 2 diabetes is a chronic condition characterized by insulin resistance and impaired insulin secretion. It is the most common form of diabetes, accounting for approximately 90-95% of all diabetes cases. Unlike type 1 diabetes, which is an autoimmune condition where the body attacks insulin-producing cells, type 2 diabetes develops gradually over time.
Causes of Type 2 Diabetes
The exact cause of type 2 diabetes is not fully understood, but several factors contribute to its development:
- Genetics: A family history of type 2 diabetes increases the risk of developing the condition.
- Obesity: Excess body fat, particularly around the abdomen, is a significant risk factor for type 2 diabetes.
- Physical Inactivity: A sedentary lifestyle can contribute to insulin resistance and type 2 diabetes.
- Unhealthy Diet: Diets high in refined carbohydrates, sugars, and unhealthy fats can increase the risk of type 2 diabetes.
- Age: The risk of type 2 diabetes increases with age, particularly after the age of 45.
- Ethnicity: Certain ethnic groups, such as African Americans, Hispanic/Latino Americans, and Native Americans, have a higher risk of developing type 2 diabetes.
- Pre-existing Conditions: Conditions such as hypertension, dyslipidemia, and polycystic ovary syndrome (PCOS) are associated with an increased risk of type 2 diabetes.
Symptoms of Type 2 Diabetes
The symptoms of type 2 diabetes are similar to those of hyperglycemia and may include:
- Increased thirst
- Frequent urination
- Fatigue
- Blurred vision
- Slow-healing sores or cuts
- Frequent infections
- Numbness or tingling in the hands or feet
Many people with type 2 diabetes may not experience noticeable symptoms initially, leading to a delayed diagnosis.
Connection Between Hyperglycemia and Type 2 Diabetes
Hyperglycemia is both a symptom and a complication of type 2 diabetes. The chronic elevation of blood sugar levels in type 2 diabetes is due to insulin resistance and impaired insulin secretion. Over time, prolonged hyperglycemia can lead to various complications and exacerbate the condition.
The Role of Insulin Resistance
Insulin resistance is a key factor in the development of type 2 diabetes. When cells in the body become resistant to insulin, the pancreas compensates by producing more insulin. Initially, this can help maintain normal blood sugar levels. However, over time, the pancreas may not be able to keep up with the increased demand for insulin, leading to hyperglycemia.
The Role of Impaired Insulin Secretion
In addition to insulin resistance, individuals with type 2 diabetes may have impaired insulin secretion. The beta cells in the pancreas that produce insulin may become dysfunctional or damaged, leading to inadequate insulin production. This further contributes to elevated blood sugar levels and the progression of type 2 diabetes.
Complications of Hyperglycemia in Type 2 Diabetes
Chronic hyperglycemia in type 2 diabetes can lead to various complications, including:
- Cardiovascular Disease: High blood sugar levels can damage blood vessels and increase the risk of heart disease, stroke, and hypertension.
- Neuropathy: Hyperglycemia can cause nerve damage, leading to peripheral neuropathy, characterized by numbness, tingling, and pain in the extremities.
- Nephropathy: Prolonged high blood sugar levels can damage the kidneys, leading to diabetic nephropathy and potential kidney failure.
- Retinopathy: Hyperglycemia can damage the blood vessels in the eyes, leading to diabetic retinopathy and vision loss.
- Foot Complications: Nerve damage and poor blood circulation can result in foot ulcers, infections, and, in severe cases, amputations.
- Skin Conditions: High blood sugar levels can increase the risk of bacterial and fungal infections and other skin conditions.
- Dental Problems: Hyperglycemia can increase the risk of gum disease and tooth decay.
Management of Hyperglycemia in Type 2 Diabetes
Managing hyperglycemia is crucial for individuals with type 2 diabetes to prevent complications and improve quality of life. Effective management involves a combination of lifestyle modifications, medications, and regular monitoring of blood sugar levels.
1. Dietary Changes
A healthy diet is fundamental in managing hyperglycemia and type 2 diabetes. Key dietary recommendations include:
- Low-Carbohydrate Diet: Reducing carbohydrate intake can help control blood sugar levels. Focus on complex carbohydrates, such as whole grains, vegetables, and legumes, while avoiding refined carbohydrates and sugars.
- Balanced Diet: Incorporate a balance of macronutrients, including lean proteins, healthy fats, and fiber-rich foods, to stabilize blood sugar levels.
- Portion Control: Eating smaller, more frequent meals can prevent blood sugar spikes and promote better glucose control.
- Avoid Sugary Foods and Beverages: Eliminate or reduce the consumption of sugary snacks, sodas, and processed foods.
2. Physical Activity
Regular physical activity is essential for managing hyperglycemia and improving insulin sensitivity. Recommendations include:
- Aerobic Exercise: Engage in at least 150 minutes of moderate-intensity aerobic exercise, such as walking, cycling, or swimming, per week.
- Strength Training: Incorporate resistance training exercises, such as weightlifting or bodyweight exercises, at least two to three times per week.
- Daily Activity: Increase daily physical activity levels by incorporating activities like walking, gardening, or taking the stairs.
3. Weight Management
Maintaining a healthy weight is crucial for managing type 2 diabetes and hyperglycemia. Strategies for weight management include:
- Caloric Deficit: Consume fewer calories than you burn to promote weight loss. Focus on nutrient-dense foods to meet nutritional needs while reducing caloric intake.
- Regular Exercise: Combine aerobic exercise, resistance training, and daily physical activity to support weight loss and improve insulin sensitivity.
- Behavioral Changes: Adopt sustainable lifestyle changes, such as mindful eating, portion control, and avoiding emotional eating, to support long-term weight management.
4. Stress Management
Chronic stress can worsen hyperglycemia and insulin resistance. Effective stress management techniques include:
- Mindfulness and Meditation: Practice mindfulness and meditation to reduce stress levels and improve overall well-being.
- Physical Activity: Engage in physical activities you enjoy, such as yoga, tai chi, or hiking, to reduce stress and improve glucose control.
- Adequate Sleep: Ensure sufficient, high-quality sleep to support stress management and overall health.
5. Medications
Medications may be necessary to manage hyperglycemia in individuals with type 2 diabetes. Common medications include:
- Metformin: A first-line medication that reduces glucose production in the liver and improves insulin sensitivity.
- Sulfonylureas: Medications that stimulate the pancreas to produce more insulin.
- DPP-4 Inhibitors: Medications that increase insulin production and reduce glucose production.
- GLP-1 Receptor Agonists: Medications that increase insulin secretion, reduce appetite, and slow gastric emptying.
- SGLT2 Inhibitors: Medications that increase glucose excretion through the urine.
6. Regular Monitoring
Regular monitoring of blood sugar levels is essential for managing hyperglycemia and type 2 diabetes. Strategies include:
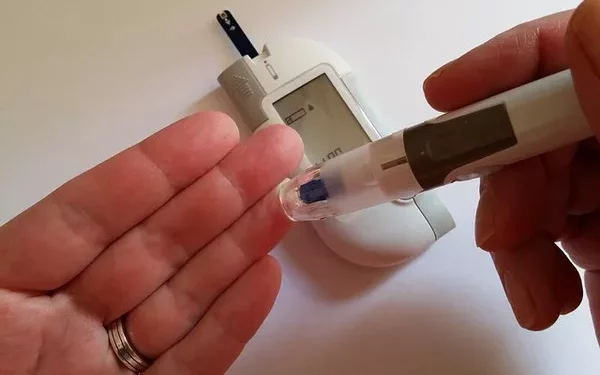
- Self-Monitoring: Use a blood glucose meter to regularly check blood sugar levels and track trends.
- Continuous Glucose Monitoring (CGM): A CGM device provides real-time blood sugar readings and trends, helping to adjust treatment and lifestyle interventions.
- Regular Check-Ups: Schedule regular check-ups with a healthcare provider to monitor blood sugar levels, assess complications, and adjust treatment plans as needed.
Prevention of Hyperglycemia and Type 2 Diabetes
Preventing hyperglycemia and type 2 diabetes involves adopting a healthy lifestyle and making proactive choices to reduce risk factors. Key preventive measures include:
1. Healthy Diet
A balanced diet rich in whole foods can help prevent hyperglycemia and type 2 diabetes. Focus on:
- Whole Grains: Choose whole grains, such as brown rice, quinoa, and oats, over refined grains.
- Fruits and Vegetables: Incorporate a variety of fruits and vegetables to provide essential nutrients and fiber.
- Lean Proteins: Include lean proteins, such as poultry, fish, beans, and legumes, to support overall health.
- Healthy Fats: Opt for healthy fats, such as avocados, nuts, seeds, and olive oil, while limiting saturated and trans fats.
- Limit Sugars and Processed Foods: Reduce the intake of sugary snacks, beverages, and processed foods to maintain stable blood sugar levels.
2. Regular Physical Activity
Engaging in regular physical activity can prevent insulin resistance and reduce the risk of type 2 diabetes. Aim for:
- Moderate-Intensity Exercise: At least 150 minutes of moderate-intensity aerobic exercise per week.
- Strength Training: Include resistance training exercises two to three times per week.
- Active Lifestyle: Incorporate physical activity into daily routines, such as walking, biking, or taking the stairs.
3. Weight Management
Maintaining a healthy weight is crucial for preventing type 2 diabetes. Strategies include:
- Balanced Diet: Consume a balanced diet with appropriate portion sizes to support a healthy weight.
- Regular Exercise: Engage in regular physical activity to maintain a healthy weight and improve insulin sensitivity.
- Behavioral Changes: Adopt sustainable lifestyle changes to support long-term weight management.
4. Stress Management
Chronic stress can contribute to insulin resistance and hyperglycemia. Effective stress management techniques include:
- Mindfulness and Meditation: Practice mindfulness and meditation to reduce stress levels.
- Physical Activity: Engage in physical activities that reduce stress and improve overall well-being.
- Adequate Sleep: Ensure sufficient, high-quality sleep to support stress management and overall health.
5. Regular Health Check-Ups
Regular health check-ups can help identify risk factors and prevent the development of type 2 diabetes. Key recommendations include:
- Blood Sugar Monitoring: Regularly check blood sugar levels to identify and address hyperglycemia early.
- Health Screenings: Schedule regular screenings for blood pressure, cholesterol, and other risk factors for type 2 diabetes.
- Consult Healthcare Providers: Work with healthcare providers to develop and maintain a personalized prevention plan.
See also: What’s Chronic Hyperglycemia
Conclusion
Hyperglycemia is a significant concern in individuals with type 2 diabetes, as it can lead to various complications and worsen the condition. Understanding the connection between hyperglycemia and type 2 diabetes is crucial for effective management and prevention. By adopting a healthy lifestyle, managing stress, and regularly monitoring blood sugar levels, individuals can prevent and manage hyperglycemia and reduce the risk of complications associated with type 2 diabetes. Collaboration with healthcare providers and adherence to personalized treatment plans are essential for achieving optimal blood sugar control and improving overall health outcomes.
Related topics:
What’s the Most Likely Cause of Hyperglycemia