Hypoglycemia, commonly known as low blood sugar, is a condition where blood glucose levels drop below normal. While diabetes is a well-known cause of hypoglycemia, it is not the only one. Various other conditions and factors can lead to hypoglycemia, which can be equally critical and demand appropriate understanding and management. This article explores the numerous causes of hypoglycemia beyond diabetes, aiming to provide a comprehensive overview for healthcare professionals and the general public.
Understanding Hypoglycemia
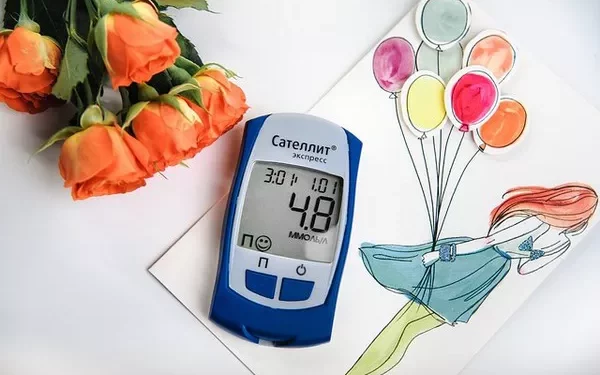
Hypoglycemia occurs when blood sugar levels fall below 70 mg/dL (3.9 mmol/L). The brain depends on glucose as its primary energy source, and when levels are too low, it can result in neurological symptoms and, in severe cases, coma or death. Symptoms of hypoglycemia can include shakiness, sweating, confusion, dizziness, hunger, irritability, and in severe cases, seizures or unconsciousness.
Causes of Hypoglycemia Beyond Diabetes
1. Medications
Various medications can induce hypoglycemia, even in non-diabetic individuals. These include:
Sulfonylureas and Insulin
Used to manage diabetes, these medications can cause hypoglycemia if taken accidentally by a non-diabetic person or if taken in excess.
Quinine
Used to treat malaria, quinine can lower blood sugar levels, especially in higher doses.
Pentamidine
An antimicrobial medication, pentamidine can induce hypoglycemia, particularly when used to treat Pneumocystis pneumonia.
Beta-blockers
While primarily used for hypertension and heart conditions, beta-blockers can mask hypoglycemia symptoms and occasionally contribute to hypoglycemia in susceptible individuals.
2. Excessive Alcohol Consumption
Alcohol-induced hypoglycemia is common in both occasional and chronic drinkers. Alcohol can impair gluconeogenesis (the production of glucose from non-carbohydrate sources) in the liver, particularly when consumed on an empty stomach or after prolonged fasting. This can lead to significant drops in blood sugar levels, sometimes dangerously so.
3. Critical Illnesses
Severe illnesses can disrupt normal glucose metabolism, leading to hypoglycemia. These include:
Sepsis
Severe infections can cause hypoglycemia due to increased glucose consumption by tissues, impaired gluconeogenesis, and diminished glycogen stores.
Hepatic Failure
The liver is crucial for glucose production and storage. Liver diseases such as hepatitis, cirrhosis, and liver failure can significantly impair these functions, leading to hypoglycemia.
Renal Failure
Kidney dysfunction can impair the clearance of hypoglycemia-inducing medications and decrease gluconeogenesis, resulting in lower blood sugar levels.
Cardiac Failure
Severe heart failure can lead to reduced cardiac output and diminished blood flow to the liver, impairing glucose production and leading to hypoglycemia.
4. Hormonal Deficiencies
Hormones play a critical role in maintaining blood glucose levels. Deficiencies in certain hormones can lead to hypoglycemia:
Adrenal Insufficiency
Cortisol is essential for glucose metabolism. Addison’s disease or adrenal insufficiency can lead to decreased cortisol levels, resulting in hypoglycemia.
Hypopituitarism
The pituitary gland regulates several hormones that influence glucose levels, including ACTH, which stimulates cortisol production. Deficiencies in these hormones can result in hypoglycemia.
Growth Hormone Deficiency
Growth hormone helps maintain blood sugar levels by stimulating gluconeogenesis. Its deficiency, particularly in children, can lead to hypoglycemia.
5. Eating Disorders and Malnutrition
Anorexia Nervosa and Bulimia Nervosa
These eating disorders can result in severe nutritional deficiencies and altered metabolism, leading to hypoglycemia due to inadequate glucose intake and glycogen stores.
Malnutrition and Starvation
Prolonged inadequate intake of calories and essential nutrients can deplete glycogen stores and reduce gluconeogenesis, leading to hypoglycemia.
6. Endocrine Tumors
Certain tumors can produce hormones or substances that affect blood glucose levels:
Insulinoma
A rare pancreatic tumor that secretes insulin independently of blood glucose levels, leading to recurrent hypoglycemia.
Non-Insulin Producing Tumors
Some tumors produce substances like insulin-like growth factors, which can mimic insulin’s effects and cause hypoglycemia.
7. Postprandial Hypoglycemia
Also known as reactive hypoglycemia, this condition occurs when blood sugar levels drop after eating. It can result from excessive insulin release following a meal. This can occur in:
Gastric Surgery
Individuals who have undergone gastric bypass or other stomach surgeries may experience rapid gastric emptying, leading to excessive insulin release and subsequent hypoglycemia.
Idiopathic Causes
In some cases, no specific cause is identified, and the condition is termed idiopathic postprandial hypoglycemia.
8. Inborn Errors of Metabolism
Certain genetic disorders can affect carbohydrate metabolism and lead to hypoglycemia:
Glycogen Storage Diseases
These genetic disorders affect the body’s ability to store and release glucose from glycogen, leading to hypoglycemia.
Galactosemia
A disorder affecting the metabolism of galactose, leading to toxic accumulation and hypoglycemia.
Hereditary Fructose Intolerance
An inability to metabolize fructose, leading to hypoglycemia upon ingestion of fructose-containing foods.
9. Physical Activity
Intensive Exercise
Prolonged and intensive physical activity can deplete glycogen stores and lower blood sugar levels, particularly if not balanced with adequate carbohydrate intake.
10. Autoimmune Hypoglycemia
Insulin Autoimmune Syndrome (Hirata’s Disease)
A rare condition where the body produces antibodies against insulin, causing spontaneous hypoglycemia.
11. Neonatal Hypoglycemia
Prematurity
Preterm infants are at risk due to inadequate glycogen stores and immature glucose regulation mechanisms.
Intrauterine Growth Restriction (IUGR)
Infants with IUGR may have reduced glycogen stores and impaired gluconeogenesis, leading to hypoglycemia.
Management and Prevention of Hypoglycemia
Managing hypoglycemia involves identifying and treating the underlying cause, monitoring blood glucose levels, and providing immediate treatment for low blood sugar episodes.
Immediate Treatment
For acute hypoglycemia, quick-acting carbohydrates such as glucose tablets, juice, or candy can raise blood sugar levels. In severe cases, intravenous glucose or glucagon injections may be necessary.
Long-Term Management
Long-term strategies focus on addressing the root cause:
Medication Review
Regularly review medications that may contribute to hypoglycemia and adjust dosages or switch medications if necessary.
Dietary Adjustments
Implementing a balanced diet with regular meals and snacks to maintain steady blood sugar levels. For conditions like reactive hypoglycemia, small, frequent meals with a balance of protein, fat, and carbohydrates can help.
Managing Underlying Conditions
Treating underlying illnesses or conditions contributing to hypoglycemia, such as hormone replacement therapy for adrenal insufficiency or surgery for insulinoma.
Education and Awareness
Educating patients and caregivers about recognizing hypoglycemia symptoms and appropriate actions to take.
See also: How Excess Sugar Intake Can Lead to Hypoglycemia
Conclusion
Hypoglycemia is a complex condition with multiple potential causes beyond diabetes. Understanding these various causes is crucial for proper diagnosis, management, and prevention. Healthcare professionals must be vigilant in identifying and addressing the underlying factors contributing to hypoglycemia to ensure effective treatment and patient safety. By doing so, the impact of hypoglycemia on individuals’ health and well-being can be minimized, promoting better overall health outcomes.
Related topics:
How Can You Prevent Hypoglycemia