Monitoring blood sugar levels is crucial for individuals with diabetes to maintain their health and prevent complications. Hypoglycemia, or low blood sugar, can be particularly dangerous if not recognized and treated promptly. This article provides an in-depth guide on how to identify the signs and symptoms of dropping blood sugar levels, the potential causes, and the steps to take to manage this condition effectively.
Understanding Blood Sugar and Hypoglycemia
Blood sugar, or glucose, is the primary energy source for the body’s cells. The body regulates blood sugar levels through various mechanisms involving hormones such as insulin and glucagon. When blood sugar levels fall below the normal range (typically below 70 mg/dL), a condition known as hypoglycemia occurs. Hypoglycemia can happen in both type 1 and type 2 diabetes patients, and recognizing its early signs is essential for timely intervention.
Symptoms of Dropping Blood Sugar
The symptoms of hypoglycemia can vary from person to person, but common signs include:
- Shakiness and Trembling: One of the first signs of low blood sugar is often a feeling of shakiness or trembling. This can occur in the hands, legs, or throughout the body.
- Sweating: Sudden sweating, especially when not related to physical activity or external temperature, can indicate a drop in blood sugar levels.
- Hunger: Intense feelings of hunger, even after recently eating, can be a symptom of low blood sugar.
- Irritability or Mood Changes: Hypoglycemia can affect the brain, leading to irritability, mood swings, or even aggressive behavior.
- Fatigue and Weakness: As the body runs low on glucose, energy levels drop, leading to fatigue and overall weakness.
- Dizziness and Lightheadedness: Low blood sugar can cause a feeling of dizziness or lightheadedness, which may lead to difficulty standing or walking.
- Confusion and Difficulty Concentrating: The brain relies heavily on glucose for proper functioning. A drop in blood sugar can cause confusion, difficulty concentrating, and poor coordination.
- Blurred Vision: Sudden changes in vision, such as blurriness or double vision, can be a sign of hypoglycemia.
- Heart Palpitations: An increased heart rate or palpitations can occur as the body tries to compensate for low blood sugar levels.
- Headaches: Persistent or severe headaches can be a symptom of hypoglycemia, especially if accompanied by other signs.
- Numbness or Tingling: Some individuals may experience numbness or a tingling sensation in their lips, tongue, or other parts of the body.
Severe Symptoms of Hypoglycemia
If blood sugar levels continue to drop without intervention, more severe symptoms can develop, including:
- Seizures: Extremely low blood sugar can cause seizures, which require immediate medical attention.
- Loss of Consciousness: Severe hypoglycemia can lead to fainting or loss of consciousness, necessitating emergency care.
- Coma: In extreme cases, untreated hypoglycemia can result in a coma, a life-threatening condition that demands urgent medical intervention.
Causes of Dropping Blood Sugar
Several factors can contribute to a drop in blood sugar levels, including:
- Medications: Insulin and certain oral diabetes medications can lower blood sugar levels. Taking too much medication or not coordinating it with food intake can lead to hypoglycemia.
- Insufficient Food Intake: Skipping meals, eating smaller portions than usual, or delaying meals can cause blood sugar levels to drop.
- Increased Physical Activity: Exercise increases glucose uptake by muscles, which can lower blood sugar levels if not balanced with food intake or medication adjustments.
- Alcohol Consumption: Alcohol can interfere with the liver’s ability to release glucose into the bloodstream, leading to hypoglycemia, especially if consumed on an empty stomach.
- Illness or Infection: Certain illnesses or infections can alter insulin requirements and affect blood sugar levels.
- Hormonal Changes: Hormonal fluctuations, particularly in women during menstrual cycles or menopause, can impact blood sugar levels.
Monitoring Blood Sugar Levels
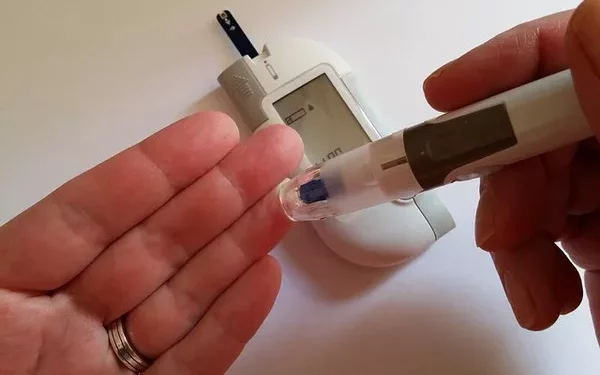
Regular monitoring of blood sugar levels is essential for preventing and managing hypoglycemia. This can be done using various methods:
- Self-Monitoring of Blood Glucose (SMBG): Using a glucometer to check blood sugar levels at home provides immediate feedback and helps in making necessary adjustments to diet, medication, or activity levels.
- Continuous Glucose Monitoring (CGM): CGM devices provide real-time blood sugar readings and trends, alerting users to rising or falling glucose levels and allowing for proactive management.
- A1C Testing: While not useful for real-time monitoring, the A1C test gives an average blood sugar level over the past two to three months and helps assess long-term glucose control.
Immediate Steps to Take if Blood Sugar is Dropping
If you suspect your blood sugar is dropping, taking immediate action is crucial:
- Check Your Blood Sugar: Use a glucometer to confirm if your blood sugar level is low.
- Consume Fast-Acting Carbohydrates: If your blood sugar is below 70 mg/dL, consume 15-20 grams of fast-acting carbohydrates, such as glucose tablets, juice, regular soda, or candies. Recheck your blood sugar after 15 minutes and repeat if necessary.
- Follow-Up with a Snack or Meal: Once your blood sugar has returned to normal, eat a small snack or meal containing protein and complex carbohydrates to maintain stable blood sugar levels.
- Adjust Medications: If you frequently experience hypoglycemia, consult with your healthcare provider to adjust your medication dosages or timing.
- Educate Those Around You: Inform family, friends, and coworkers about the signs of hypoglycemia and how they can assist you if needed.
Preventing Hypoglycemia
Prevention is key to managing diabetes and avoiding the dangers of hypoglycemia. Here are some strategies to help prevent low blood sugar levels:
- Regular Monitoring: Keep track of your blood sugar levels regularly to identify patterns and make necessary adjustments to your diabetes management plan.
- Consistent Eating Schedule: Maintain a consistent eating schedule and include balanced meals and snacks to stabilize blood sugar levels.
- Coordinate Medication and Food Intake: Ensure that your medication regimen aligns with your meals and snacks to prevent blood sugar fluctuations.
- Adjust for Physical Activity: Monitor blood sugar levels before, during, and after physical activity, and adjust food intake or medication as needed.
- Limit Alcohol Consumption: If you choose to drink alcohol, do so in moderation and always with food to prevent hypoglycemia.
- Educate Yourself: Stay informed about diabetes management and the potential triggers of hypoglycemia. Knowledge is a powerful tool in preventing and managing low blood sugar.
When to Seek Medical Attention
While many episodes of hypoglycemia can be managed at home, there are times when medical attention is necessary:
- Frequent Hypoglycemia: If you experience frequent episodes of low blood sugar, consult with your healthcare provider to review and adjust your diabetes management plan.
- Severe Symptoms: Seek emergency medical help if you or someone else experiences severe symptoms of hypoglycemia, such as seizures, loss of consciousness, or an inability to swallow.
- Unexplained Hypoglycemia: If you cannot identify the cause of your low blood sugar levels, work with your healthcare team to uncover potential underlying issues.
See also: What’s the Best CGMs for Type 2 Diabetes
Conclusion
Recognizing the signs of dropping blood sugar levels and understanding how to respond is vital for individuals with diabetes. By staying vigilant, monitoring blood sugar levels regularly, and maintaining a well-balanced diet and medication regimen, you can effectively manage hypoglycemia and maintain optimal health. Always consult with your healthcare provider for personalized advice and adjustments to your diabetes management plan.
Related topics:
What’s the Best Accu-Chek Meter