Insulin resistance is a metabolic condition where the body’s cells become less responsive to the hormone insulin, leading to impaired glucose uptake and increased blood sugar levels. This condition is a precursor to type 2 diabetes and is often associated with other metabolic disorders, such as obesity, hypertension, and dyslipidemia. Understanding the pathophysiology of insulin resistance is crucial for identifying risk factors, implementing preventive measures, and managing the condition effectively. This article will explore the biochemical mechanisms underlying insulin resistance, its impact on various body systems, and potential treatment strategies.
Understanding Insulin and Its Role
Insulin Production and Function
Insulin is a hormone produced by the beta cells in the islets of Langerhans in the pancreas. It plays a vital role in regulating blood glucose levels by facilitating the uptake of glucose into cells, particularly in the liver, muscle, and adipose tissues. Insulin promotes glucose storage as glycogen in the liver and muscle cells, inhibits gluconeogenesis (the production of glucose from non-carbohydrate sources), and prevents the breakdown of fat for energy.
Insulin Signaling Pathway
The insulin signaling pathway involves a series of complex biochemical reactions. When insulin binds to its receptor on the cell surface, it triggers a cascade of events that result in the translocation of glucose transporter type 4 (GLUT4) to the cell membrane. GLUT4 facilitates the entry of glucose into the cell, thus reducing blood glucose levels. This pathway is tightly regulated and involves multiple proteins and enzymes, including insulin receptor substrate (IRS), phosphoinositide 3-kinase (PI3K), and protein kinase B (Akt).
Pathophysiology of Insulin Resistance
Impaired Insulin Signaling
In insulin resistance, the signaling pathway is disrupted, leading to decreased glucose uptake by cells. This impairment can occur at various levels, including the insulin receptor, IRS, PI3K, and Akt. One common issue is the phosphorylation of serine residues on IRS instead of tyrosine residues, which inhibits its activity and downstream signaling. Factors contributing to this disruption include chronic inflammation, oxidative stress, and the accumulation of lipid metabolites.
Role of Adipose Tissue
Adipose tissue plays a critical role in the development of insulin resistance. Excessive fat accumulation, particularly in visceral adipose tissue, leads to the release of free fatty acids (FFAs) and pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6). These substances interfere with insulin signaling and promote a state of chronic low-grade inflammation, which further exacerbates insulin resistance.
Inflammation and Oxidative Stress
Chronic inflammation and oxidative stress are key contributors to insulin resistance. Inflammatory cytokines activate stress-related signaling pathways, such as the c-Jun N-terminal kinase (JNK) and IκB kinase (IKK) pathways, which phosphorylate IRS on serine residues, inhibiting its activity. Oxidative stress, characterized by an imbalance between reactive oxygen species (ROS) and antioxidant defenses, also damages cellular components and disrupts insulin signaling.
Lipid Metabolism and Ectopic Fat Deposition
Dysregulated lipid metabolism is another crucial factor in insulin resistance. Elevated levels of FFAs can impair insulin signaling in liver and muscle cells. Additionally, the accumulation of lipid intermediates, such as diacylglycerol (DAG) and ceramides, in non-adipose tissues (ectopic fat deposition) can directly inhibit insulin signaling pathways. This is particularly evident in conditions like non-alcoholic fatty liver disease (NAFLD) and muscle insulin resistance.
Impact on Various Body Systems
Muscle Tissue
Muscle tissue is a major site for glucose uptake, and insulin resistance in muscle cells significantly impacts overall glucose homeostasis. Impaired glucose uptake in muscle cells results in elevated blood glucose levels, leading to hyperglycemia. This can cause a shift in energy metabolism, where the muscle cells increasingly rely on fatty acids for energy, further exacerbating lipid accumulation and insulin resistance.
Liver
The liver plays a central role in glucose metabolism by regulating glycogen storage and gluconeogenesis. In insulin resistance, the liver becomes resistant to the inhibitory effects of insulin on glucose production. As a result, gluconeogenesis continues unchecked, contributing to elevated blood glucose levels. Additionally, insulin resistance in the liver is associated with increased lipogenesis (fat synthesis) and the development of NAFLD, which further impairs insulin sensitivity.
Adipose Tissue
Adipose tissue not only stores fat but also acts as an endocrine organ, secreting various adipokines that influence insulin sensitivity. In insulin resistance, there is an imbalance in adipokine secretion, with reduced levels of adiponectin (an insulin-sensitizing hormone) and increased levels of leptin and pro-inflammatory cytokines. This dysregulation contributes to systemic inflammation and further impairs insulin signaling.
Pancreas
As insulin resistance progresses, the pancreas compensates by increasing insulin production to maintain normal blood glucose levels. This compensatory hyperinsulinemia can eventually lead to beta-cell dysfunction and failure. The prolonged demand for insulin production stresses the beta cells, leading to their exhaustion and apoptosis. This decline in beta-cell function marks the transition from insulin resistance to type 2 diabetes.
Cardiovascular System
Insulin resistance is closely linked to cardiovascular diseases (CVD). The condition is often associated with a cluster of risk factors known as metabolic syndrome, which includes hypertension, dyslipidemia, and central obesity. Insulin resistance contributes to endothelial dysfunction, increased arterial stiffness, and the development of atherosclerosis, all of which elevate the risk of cardiovascular events such as heart attack and stroke.
Kidneys
Insulin resistance also affects renal function. Hyperinsulinemia and hyperglycemia can lead to glomerular hyperfiltration and increased renal sodium reabsorption, contributing to hypertension. Over time, the high glucose levels damage the glomeruli, leading to diabetic nephropathy, a major cause of end-stage renal disease.
Factors Contributing to Insulin Resistance
Genetic Predisposition
Genetics play a significant role in determining an individual’s susceptibility to insulin resistance. Certain gene variants are associated with impaired insulin signaling and glucose metabolism. Family history of type 2 diabetes and related metabolic disorders increases the risk of developing insulin resistance.
Obesity
Obesity, particularly central obesity, is a major risk factor for insulin resistance. Excess adipose tissue, especially visceral fat, secretes FFAs and inflammatory cytokines that disrupt insulin signaling. The accumulation of ectopic fat in organs such as the liver and muscle further exacerbates insulin resistance.
Physical Inactivity
Lack of physical activity contributes to the development of insulin resistance. Regular exercise enhances insulin sensitivity by promoting glucose uptake in muscle cells and improving mitochondrial function. Sedentary behavior, on the other hand, leads to decreased muscle mass and increased fat accumulation, impairing glucose metabolism.
Unhealthy Diet
A diet high in refined carbohydrates, sugars, and unhealthy fats promotes insulin resistance. These dietary components can lead to obesity, increased FFA levels, and chronic inflammation. Conversely, a diet rich in whole grains, lean proteins, healthy fats, and fiber supports insulin sensitivity and overall metabolic health.
Hormonal Imbalances
Certain hormonal conditions, such as polycystic ovary syndrome (PCOS) and Cushing’s syndrome, are associated with insulin resistance. These conditions involve hormonal imbalances that can affect glucose metabolism and insulin sensitivity.
Sleep Disorders
Sleep disorders, including sleep apnea and chronic sleep deprivation, are linked to insulin resistance. Poor sleep quality and duration can disrupt hormonal regulation and increase stress hormones such as cortisol, which impair insulin signaling.
Chronic Stress
Chronic stress contributes to insulin resistance through the activation of the hypothalamic-pituitary-adrenal (HPA) axis and the release of stress hormones like cortisol. These hormones interfere with insulin signaling and promote glucose production, leading to elevated blood glucose levels.
Diagnosis of Insulin Resistance
Clinical Assessment
Diagnosing insulin resistance involves a combination of clinical assessment, laboratory tests, and identifying associated risk factors. Clinical assessment includes evaluating the patient’s medical history, family history, and physical examination, with particular attention to signs of obesity, acanthosis nigricans (dark, thickened skin patches), and metabolic syndrome features.
Laboratory Tests
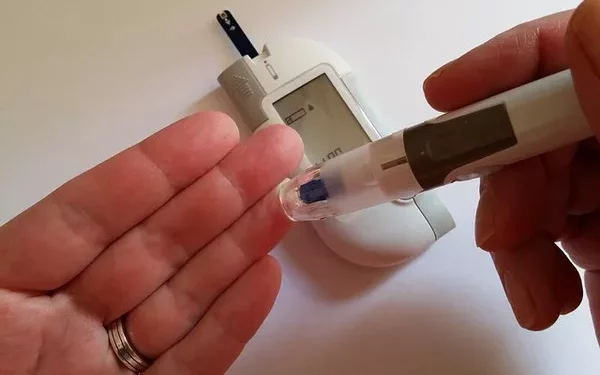
Several laboratory tests are used to assess insulin resistance and its impact on glucose metabolism:
- Fasting Blood Glucose: Measures blood glucose levels after an overnight fast. Elevated levels may indicate insulin resistance or diabetes.
- Oral Glucose Tolerance Test (OGTT): Evaluates the body’s ability to handle glucose over a specified period. It involves fasting blood glucose measurement followed by consuming a glucose-rich drink and subsequent blood glucose measurements.
- Hemoglobin A1c (HbA1c): Reflects average blood glucose levels over the past 2-3 months. Elevated HbA1c levels suggest poor long-term glucose control.
- Fasting Insulin Levels: High fasting insulin levels indicate compensatory hyperinsulinemia due to insulin resistance.
- Homeostatic Model Assessment of Insulin Resistance (HOMA-IR): A mathematical model that estimates insulin resistance based on fasting glucose and insulin levels.
Advanced Diagnostic Tools
In some cases, advanced diagnostic tools such as hyperinsulinemic-euglycemic clamp and frequently sampled intravenous glucose tolerance test (FSIVGTT) may be used in research settings to provide more precise measurements of insulin sensitivity.
Management of Insulin Resistance
Lifestyle Modifications
Lifestyle modifications are the cornerstone of managing insulin resistance. These include:
- Healthy Diet: Adopting a balanced diet rich in whole grains, lean proteins, healthy fats, and fiber. Reducing the intake of refined sugars, processed foods, and unhealthy fats.
- Regular Exercise: Engaging in regular physical activity, including aerobic exercise and resistance training, to enhance insulin sensitivity and promote weight loss.
- Weight Management: Achieving and maintaining a healthy weight through diet and exercise. Even modest weight loss can significantly improve insulin sensitivity.
- Stress Management: Implementing stress-reduction techniques such as mindfulness, meditation, and yoga to reduce the impact of chronic stress on insulin resistance.
- Adequate Sleep: Ensuring sufficient and quality sleep to support metabolic health and hormone regulation.
Pharmacological Interventions
In some cases, pharmacological interventions may be necessary to manage insulin resistance and prevent the progression to type 2 diabetes:
- Metformin: A commonly prescribed medication that improves insulin sensitivity and reduces hepatic glucose production. It is often used in patients with prediabetes or early type 2 diabetes.
- Thiazolidinediones (TZDs): A class of medications that enhance insulin sensitivity in adipose tissue and muscle. Examples include pioglitazone and rosiglitazone.
- GLP-1 Receptor Agonists: Medications that mimic the action of the incretin hormone GLP-1, which enhances insulin secretion and promotes satiety. Examples include liraglutide and exenatide.
- SGLT2 Inhibitors: Medications that inhibit the reabsorption of glucose in the kidneys, leading to increased glucose excretion in the urine. Examples include canagliflozin and dapagliflozin.
Monitoring and Follow-Up
Regular monitoring and follow-up are essential for managing insulin resistance and preventing complications. This includes routine blood glucose and HbA1c measurements, lipid profile assessments, and periodic evaluation of kidney and liver function. Patients should also be educated about the importance of adherence to lifestyle modifications and medication regimens.
See also: What are Insulin Resistance’s Diagnosis and Implications
Conclusion
Insulin resistance is a complex metabolic condition with far-reaching effects on various body systems. It involves impaired insulin signaling, chronic inflammation, and dysregulated lipid metabolism, leading to hyperglycemia and an increased risk of type 2 diabetes and cardiovascular diseases. Effective management of insulin resistance requires a comprehensive approach, including lifestyle modifications, pharmacological interventions, and regular monitoring. By addressing the underlying factors contributing to insulin resistance, healthcare providers can help patients improve their metabolic health and reduce the risk of long-term complications.
Related topics:
How Insulin Resistance Causes Pcos
What’s the Link Between Insulin Resistance and Hypertension
What’s the relationship of Insulin Resistance and Heart Disease