Hypoglycemia, characterized by abnormally low blood glucose levels, is a critical condition requiring immediate attention. It is particularly concerning for individuals with diabetes, as it can lead to severe complications if not managed promptly. While diet, physical activity, and overall health play significant roles in blood glucose regulation, medication remains a pivotal factor. Certain medications, prescribed primarily for diabetes management, can cause hypoglycemia as a side effect. This article delves into these medications, exploring their mechanisms, effects, and strategies for managing and preventing hypoglycemia.
Mechanisms of Hypoglycemia
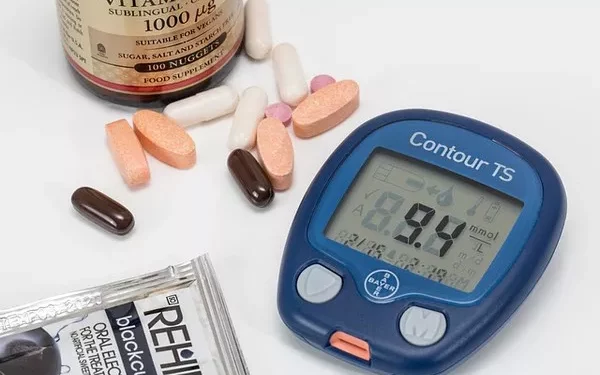
Hypoglycemia occurs when blood glucose levels fall below the normal range, typically below 70 mg/dL. The brain and other organs rely on glucose as a primary energy source, and a deficiency can lead to symptoms ranging from mild discomfort to severe neurological impairments. Common symptoms include shakiness, sweating, confusion, and in severe cases, loss of consciousness or seizures.
The regulation of blood glucose involves a delicate balance between insulin, which lowers blood glucose, and counter-regulatory hormones like glucagon, epinephrine, cortisol, and growth hormone, which raise it. Medications that interfere with this balance, either by increasing insulin levels or decreasing the production of counter-regulatory hormones, can lead to hypoglycemia.
Medications Causing Hypoglycemia
1. Insulin
Insulin therapy is a cornerstone of diabetes management, particularly for individuals with Type 1 diabetes and for some with Type 2 diabetes. Insulin is administered through injections or an insulin pump to help manage blood glucose levels. However, inappropriate dosing or timing of insulin administration can cause hypoglycemia.
Types of Insulin:
Rapid-acting insulin: Includes aspart, lispro, and glulisine. They start working within 15 minutes, peak at 1-2 hours, and last for 3-5 hours.
Short-acting insulin: Regular insulin, which begins to work within 30 minutes, peaks at 2-3 hours, and lasts for 5-8 hours.
Intermediate-acting insulin: NPH insulin, which starts working in 1-2 hours, peaks at 4-12 hours, and lasts for 18-24 hours.
Long-acting insulin: Includes glargine, detemir, and degludec. They have a prolonged duration of action with little to no peak, lasting up to 24 hours or more.
Mechanism:
Insulin facilitates the uptake of glucose by tissues and inhibits glucose production by the liver. Overdosing insulin or mismatching insulin administration with food intake or physical activity can lead to excessive glucose uptake and hypoglycemia.
Management:
Educate patients on insulin timing and dose adjustments.
Frequent monitoring of blood glucose levels.
Adjusting insulin doses based on carbohydrate intake and physical activity.
2. Sulfonylureas
Sulfonylureas are oral medications used to manage Type 2 diabetes. They stimulate the pancreas to release more insulin, thereby lowering blood glucose levels.
Examples:
First-generation: Chlorpropamide, tolbutamide.
Second-generation: Glipizide, glyburide, glimepiride.
Mechanism:
Sulfonylureas bind to specific receptors on pancreatic beta cells, causing depolarization and an influx of calcium ions, which stimulates insulin release. However, if insulin secretion exceeds the body’s requirement, it can result in hypoglycemia.
Risk Factors:
Long duration of action, particularly with glyburide.
Renal impairment, leading to decreased drug clearance.
Elderly patients, due to reduced renal function and polypharmacy.
Management:
Use the lowest effective dose.
Prefer short-acting agents in elderly patients.
Monitor renal function and adjust doses accordingly.
3. Meglitinides
Meglitinides, like sulfonylureas, stimulate insulin secretion from the pancreas but have a shorter duration of action.
Examples:
Repaglinide
Nateglinide
Mechanism:
Meglitinides close ATP-dependent potassium channels in beta cells, leading to depolarization and calcium influx, which stimulates insulin release. Due to their rapid onset and short duration, they are taken before meals to manage postprandial glucose levels.
Risk Factors:
Missed meals or irregular eating patterns can increase the risk of hypoglycemia.
Management:
Take meglitinides before meals.
Skip the dose if a meal is skipped to avoid hypoglycemia.
4. GLP-1 Receptor Agonists and DPP-4 Inhibitors
Glucagon-like peptide-1 (GLP-1) receptor agonists and dipeptidyl peptidase-4 (DPP-4) inhibitors are newer classes of diabetes medications that enhance the incretin effect.
Examples:
GLP-1 Receptor Agonists: Exenatide, liraglutide, dulaglutide.
DPP-4 Inhibitors: Sitagliptin, saxagliptin, linagliptin.
Mechanism:
GLP-1 receptor agonists mimic the action of the incretin hormone GLP-1, which enhances glucose-dependent insulin secretion, suppresses glucagon release, and slows gastric emptying. DPP-4 inhibitors prevent the breakdown of incretins, thereby prolonging their action. These medications typically have a low risk of hypoglycemia when used alone but can cause hypoglycemia when combined with other hypoglycemic agents, particularly sulfonylureas or insulin.
Management:
Consider dose adjustments of concomitant insulin or sulfonylureas.
Educate patients about recognizing hypoglycemia symptoms, especially when using combination therapy.
5. SGLT2 Inhibitors
Sodium-glucose co-transporter 2 (SGLT2) inhibitors are a class of medications that lower blood glucose by preventing glucose reabsorption in the kidneys.
Examples:
Canagliflozin
Dapagliflozin
Empagliflozin
Mechanism:
SGLT2 inhibitors block the reabsorption of glucose in the proximal tubules of the kidneys, leading to increased glucose excretion in the urine. While they typically do not cause hypoglycemia on their own, they can increase the risk when used in combination with insulin or insulin secretagogues.
Management:
Monitor blood glucose levels regularly.
Adjust doses of concomitant medications to minimize hypoglycemia risk.
Educate patients on the importance of hydration and recognizing signs of hypoglycemia.
Non-Diabetic Medications Causing Hypoglycemia
While diabetes medications are the primary culprits, other medications can also induce hypoglycemia, particularly in vulnerable populations.
1. Quinine
Quinine, used primarily for treating malaria, can cause hypoglycemia by stimulating insulin secretion.
Mechanism:
Quinine increases insulin secretion by the pancreas, which can lead to hypoglycemia, particularly in individuals with impaired glucose counter-regulation.
Management:
Monitor blood glucose levels in patients receiving quinine therapy.
Educate patients about the potential for hypoglycemia and its symptoms.
2. Beta-Blockers
Beta-blockers are used to manage cardiovascular conditions like hypertension and arrhythmias. They can mask hypoglycemia symptoms and, in some cases, contribute to hypoglycemia.
Examples:
Propranolol
Metoprolol
Mechanism:
Beta-blockers inhibit the action of catecholamines, which are part of the counter-regulatory response to hypoglycemia. They can also impair glycogenolysis and gluconeogenesis, leading to hypoglycemia.
Risk Factors:
Non-selective beta-blockers (e.g., propranolol) pose a higher risk than selective ones (e.g., metoprolol).
Management:
Use cardioselective beta-blockers in patients with diabetes.
Educate patients on the signs of hypoglycemia and the potential masking effect of beta-blockers.
3. Pentamidine
Pentamidine is an antiprotozoal medication used to treat Pneumocystis pneumonia, particularly in immunocompromised patients.
Mechanism:
Pentamidine can cause both hyperglycemia and hypoglycemia by damaging pancreatic beta cells, leading to insulin release and subsequent hypoglycemia.
Management:
Monitor blood glucose levels closely in patients receiving pentamidine.
Be vigilant for both hypoglycemia and hyperglycemia during and after treatment.
Preventing Hypoglycemia
Preventing hypoglycemia involves a multifaceted approach, including patient education, regular monitoring, and individualized treatment plans.
1. Patient Education
Educating patients about hypoglycemia is critical. This includes recognizing symptoms, understanding the impact of medications, and knowing how to respond to low blood glucose levels.
Key Points:
Teach patients to monitor blood glucose levels regularly.
Encourage carrying glucose tablets or a quick source of sugar.
Educate on the importance of regular meals and snacks.
2. Regular Monitoring
Frequent blood glucose monitoring helps detect hypoglycemia early and allows for timely intervention.
Strategies:
Self-monitoring of blood glucose (SMBG) at home.
Continuous glucose monitoring (CGM) systems for real-time data.
3. Individualized Treatment Plans
Tailoring treatment plans to individual needs can minimize the risk of hypoglycemia.
Considerations:
Adjust medication doses based on lifestyle, dietary habits, and activity levels.
Choose medications with a lower risk of hypoglycemia for high-risk patients.
See also: What Level of Blood Sugar is Dangerous Hypoglycemia
Conclusion
Hypoglycemia is a significant concern for individuals managing diabetes, especially those on medications that influence blood glucose levels. Understanding the medications that cause hypoglycemia, their mechanisms, and how to manage the risk is crucial for healthcare providers and patients alike. Through patient education, regular monitoring, and individualized treatment plans, the risk of hypoglycemia can be effectively managed, ensuring better outcomes and quality of life for those affected.
By staying informed and proactive, healthcare providers can help patients navigate the complexities of diabetes management, minimizing the risk of hypoglycemia and its potentially severe consequences.
Related topics:
What Is The Definition Of Hypoglycemia?