Pregnancy is a unique and complex physiological state that requires careful monitoring of various health parameters to ensure the well-being of both the mother and the developing fetus. One critical aspect of maternal health is the maintenance of appropriate blood sugar levels. While much attention is often given to high blood sugar levels and gestational diabetes, low blood sugar (hypoglycemia) during pregnancy is also a significant concern that can have profound implications. This article delves into the causes, symptoms, risks, and management strategies for low blood sugar during pregnancy, aiming to provide a comprehensive understanding of this condition.
What is Hypoglycemia?
Hypoglycemia is a condition characterized by abnormally low levels of glucose in the blood. Glucose is a primary energy source for the body, and maintaining its levels within a specific range is essential for proper bodily function. In non-pregnant individuals, blood sugar levels are typically maintained through a balance between food intake, insulin secretion, and glucose production by the liver. However, during pregnancy, this balance can be disrupted due to various physiological changes.
Causes of Hypoglycemia in Pregnancy
Increased Insulin Sensitivity: Pregnancy induces several hormonal changes, one of which is increased sensitivity to insulin. This can lead to more rapid and efficient utilization of glucose by the body’s cells, potentially resulting in lower blood glucose levels.
Increased Metabolic Demands: The growing fetus requires a significant amount of glucose for development. This increased metabolic demand can sometimes outpace the mother’s glucose production, leading to hypoglycemia.
Nutritional Factors: Inadequate caloric intake, particularly if meals are skipped or not nutritionally balanced, can lead to low blood sugar levels. Morning sickness and severe nausea can also contribute to reduced food intake, exacerbating the risk of hypoglycemia.
Exercise: Physical activity increases glucose utilization by muscles. While exercise is generally beneficial during pregnancy, excessive or poorly timed exercise can lead to hypoglycemia, especially if not compensated with adequate nutrition.
Pre-existing Conditions: Women with pre-existing diabetes who are on insulin therapy are at increased risk of hypoglycemia, particularly if their insulin doses are not appropriately adjusted during pregnancy.
Symptoms of Hypoglycemia
The symptoms of hypoglycemia can range from mild to severe and can vary between individuals. Common symptoms include:
Mild Hypoglycemia:
- Shakiness or trembling
- Sweating
- Hunger
- Dizziness or lightheadedness
- Rapid heartbeat
- Irritability or mood changes
Moderate Hypoglycemia:
- Confusion or difficulty concentrating
- Weakness or fatigue
- Blurred vision
- Headache
- Clumsiness or lack of coordination
Severe Hypoglycemia:
- Seizures
- Loss of consciousness
- Coma
It is crucial for pregnant women to recognize these symptoms early and take appropriate action to prevent progression to more severe hypoglycemia.
Risks Associated with Hypoglycemia in Pregnancy
Maternal Risks:
- Physical Injuries: Severe hypoglycemia can lead to fainting or seizures, increasing the risk of physical injuries from falls.
- Impaired Cognitive Function: Frequent episodes of hypoglycemia can impair cognitive function and daily activities.
- Psychological Impact: The constant fear of hypoglycemic episodes can lead to anxiety and reduced quality of life.
Fetal Risks:
- Intrauterine Growth Restriction (IUGR): Chronic hypoglycemia can impair placental function and nutrient delivery to the fetus, leading to IUGR.
- Preterm Birth: Severe maternal hypoglycemia can increase the risk of preterm labor.
- Neurodevelopmental Issues: There is some evidence to suggest that severe or recurrent maternal hypoglycemia may impact fetal brain development, potentially leading to neurodevelopmental issues.
Diagnosing Hypoglycemia in Pregnancy
Diagnosis of hypoglycemia involves both clinical evaluation and laboratory testing. Key steps include:
Clinical History: Detailed history taking to identify symptoms, frequency, and triggers of hypoglycemia.
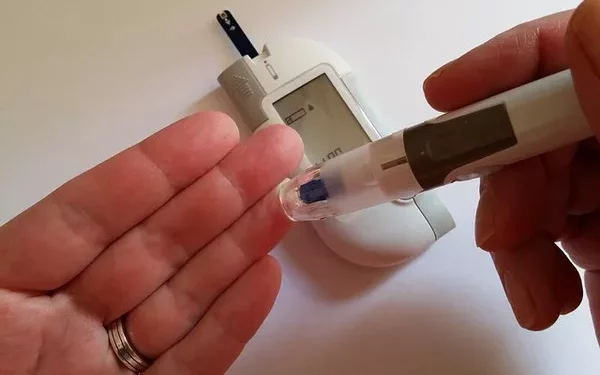
Blood Glucose Monitoring: Regular monitoring of blood glucose levels using a glucometer. This is especially important for women with diabetes or those experiencing frequent symptoms.
Continuous Glucose Monitoring (CGM): For more detailed insights, a CGM device can provide continuous readings of blood glucose levels throughout the day and night, helping to identify patterns and prevent episodes.
Management Strategies
Managing hypoglycemia during pregnancy involves a combination of dietary adjustments, lifestyle modifications, and medical interventions when necessary. Key strategies include:
Nutritional Management:
- Frequent Small Meals: Eating small, balanced meals and snacks throughout the day can help maintain stable blood sugar levels.
- Complex Carbohydrates: Including complex carbohydrates with a low glycemic index in the diet can provide a steady release of glucose into the bloodstream.
- Protein and Fiber: Adding protein and fiber to meals can slow the absorption of glucose and prevent rapid blood sugar fluctuations.
- Avoiding Sugary Foods: While sugary foods can cause a rapid spike in blood glucose, they can also lead to subsequent crashes. It is better to avoid them in favor of more balanced options.
Lifestyle Modifications:
- Regular Monitoring: Frequent self-monitoring of blood glucose levels can help detect early signs of hypoglycemia and prompt timely intervention.
- Physical Activity: Engaging in regular, moderate exercise is beneficial, but it should be well-timed with meals and snacks to prevent hypoglycemia.
- Stress Management: Reducing stress through relaxation techniques, adequate sleep, and support systems can help maintain stable blood glucose levels.
Medical Interventions:
- Insulin Adjustment: For women with diabetes, insulin doses may need to be adjusted more frequently during pregnancy to account for changing insulin sensitivity and metabolic demands.
- Medication Review: Any medications that can influence blood sugar levels should be reviewed and adjusted as necessary.
- Emergency Measures: In cases of severe hypoglycemia, having a glucagon kit available can be lifesaving. Glucagon is a hormone that quickly raises blood glucose levels and can be administered by a caregiver in emergencies.
Preventing Hypoglycemia During Pregnancy
Prevention of hypoglycemia during pregnancy is paramount and involves a proactive approach to health management. Key preventive measures include:
Preconception Counseling: For women with pre-existing diabetes, preconception counseling and optimization of blood glucose control before pregnancy can reduce the risk of hypoglycemia.
Individualized Care Plans: Each pregnancy is unique, and care plans should be tailored to the individual needs of the mother, taking into account her medical history, lifestyle, and pregnancy progression.
Education and Support: Educating pregnant women about the signs, symptoms, and management of hypoglycemia can empower them to take control of their health. Support from healthcare providers, family, and support groups is also essential.
Regular Prenatal Visits: Frequent prenatal visits allow for continuous monitoring of maternal and fetal health, enabling early detection and management of any issues, including hypoglycemia.
Special Considerations for Women with Diabetes
Women with pre-existing diabetes are at higher risk of both hyperglycemia and hypoglycemia during pregnancy. Special considerations for these women include:
Tight Glycemic Control: Maintaining tight glycemic control is crucial to prevent both high and low blood sugar levels. This often requires more frequent blood glucose monitoring and insulin adjustments.
Preconception Planning: Optimizing blood glucose control before conception can reduce the risk of complications during pregnancy.
Advanced Monitoring Tools: Utilizing advanced glucose monitoring tools like CGM can provide detailed insights into glucose patterns and help prevent hypoglycemic episodes.
Coordination of Care: A multidisciplinary care team, including obstetricians, endocrinologists, and diabetes educators, can provide comprehensive care and support for women with diabetes during pregnancy.
Long-term Outlook and Postpartum Considerations
The management of hypoglycemia does not end with pregnancy. Postpartum considerations are equally important to ensure the ongoing health of both the mother and the child. Key aspects include:
Postpartum Blood Glucose Monitoring: Continued monitoring of blood glucose levels postpartum is essential, especially for women with diabetes or those who experienced significant hypoglycemia during pregnancy.
Breastfeeding and Nutrition: Breastfeeding mothers need to maintain adequate nutrition to prevent hypoglycemia, as lactation increases caloric and glucose demands.
Postpartum Follow-up: Regular follow-up appointments with healthcare providers can help manage any lingering issues and ensure a smooth transition to postpartum life.
See also: What Will Lower Blood Sugar Immediately
Conclusion
Low blood sugar during pregnancy is a critical concern that requires vigilant monitoring and management to ensure the health and safety of both the mother and the developing fetus. Understanding the causes, symptoms, risks, and management strategies for hypoglycemia is essential for healthcare providers and pregnant women alike. By adopting a proactive approach and individualized care plans, the risks associated with hypoglycemia can be effectively mitigated, leading to positive outcomes for both mother and child.
Related topics:
What Indicates Gestational Diabetes