Type 2 diabetes mellitus (T2DM) is a chronic metabolic disorder characterized by insulin resistance and relative insulin deficiency. Managing this condition effectively requires a multifaceted approach that typically begins with lifestyle modifications and the administration of metformin, the first-line pharmacological treatment. Metformin is well-documented for its efficacy in lowering HbA1c levels, improving insulin sensitivity, and promoting weight loss. However, as the disease progresses, many patients find that metformin alone is insufficient to maintain optimal glycemic control. This necessitates the addition of other therapeutic agents to achieve target HbA1c levels and prevent complications associated with T2DM.
The Importance of Glycemic Control in T2DM
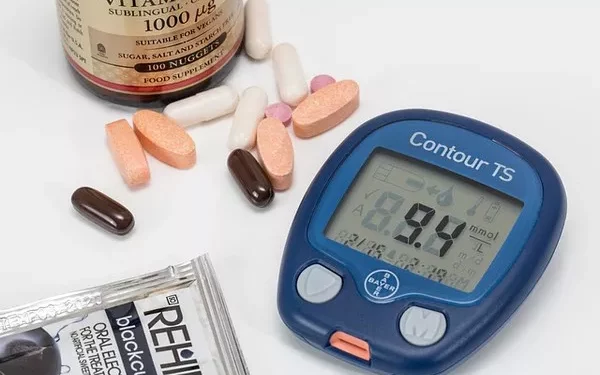
Maintaining glycemic control is crucial in the management of T2DM to prevent both microvascular and macrovascular complications. The HbA1c test, which measures the average blood glucose levels over the past two to three months, is a key marker used to assess the effectiveness of diabetes management. The American Diabetes Association (ADA) recommends an HbA1c target of less than 7% for most adults with T2DM, though individual targets may vary based on factors such as age, comorbidities, and risk of hypoglycemia.
Why Metformin Alone May Not Be Enough
Metformin is often the first-line treatment due to its efficacy, safety profile, and benefits beyond glucose control, including cardiovascular protection. However, its effectiveness can diminish over time as the disease progresses. This decline in efficacy is partly due to the progressive nature of T2DM, which involves increasing insulin resistance and beta-cell dysfunction. When metformin alone is insufficient to achieve glycemic targets, additional pharmacological interventions are required.
Options for Adding to Metformin Therapy
When intensifying treatment for patients who are not achieving their HbA1c targets on metformin alone, several classes of medications can be considered. These include sulfonylureas, thiazolidinediones, DPP-4 inhibitors, GLP-1 receptor agonists, SGLT2 inhibitors, and insulin. The choice of an additional agent should be individualized based on the patient’s characteristics, comorbidities, risk of adverse effects, and preferences.
Sulfonylureas
Mechanism of Action:
Sulfonylureas stimulate insulin secretion from pancreatic beta cells. They are effective at lowering HbA1c by 1-2%.
Advantages:
- Cost-effective
- Widely available
- Rapid reduction in blood glucose levels
Disadvantages:
- Risk of hypoglycemia
- Potential for weight gain
- Reduced effectiveness over time due to beta-cell burnout
Clinical Considerations:
Sulfonylureas may be particularly useful in patients with no history of severe hypoglycemia and those who require a rapid reduction in blood glucose levels. However, their use should be cautious in patients with cardiovascular disease or those at high risk of hypoglycemia.
Thiazolidinediones (TZDs)
Mechanism of Action:
TZDs improve insulin sensitivity by activating peroxisome proliferator-activated receptor gamma (PPAR-γ). They reduce HbA1c by approximately 0.5-1.4%.
Advantages:
- Improvement in insulin sensitivity
- Durability in glucose-lowering effect
- Potential benefits on lipid profiles
Disadvantages:
- Weight gain
- Risk of fluid retention and heart failure
- Increased risk of fractures
- Potential increase in cardiovascular risk with certain TZDs
Clinical Considerations:
TZDs may be considered for patients with significant insulin resistance and no history of heart failure or osteoporosis. Pioglitazone, in particular, has shown potential cardiovascular benefits in some studies.
DPP-4 Inhibitors
Mechanism of Action:
DPP-4 inhibitors enhance the incretin system, leading to increased insulin release and decreased glucagon secretion. They lower HbA1c by 0.5-1%.
Advantages:
- Low risk of hypoglycemia
- Weight-neutral
- Oral administration
Disadvantages:
- Modest efficacy in reducing HbA1c
- Potential for joint pain
- Rare cases of pancreatitis
Clinical Considerations:
DPP-4 inhibitors are suitable for patients who require modest HbA1c reduction and are at risk of hypoglycemia or weight gain. They are also an option for those who prefer oral medications over injections.
GLP-1 Receptor Agonists
Mechanism of Action:
GLP-1 receptor agonists mimic the incretin hormone GLP-1, stimulating insulin secretion, inhibiting glucagon release, slowing gastric emptying, and promoting satiety. They lower HbA1c by 0.5-1.5%.
Advantages:
- Significant HbA1c reduction
- Weight loss
- Cardiovascular benefits (e.g., liraglutide, semaglutide)
- Low risk of hypoglycemia
Disadvantages:
- Gastrointestinal side effects (nausea, vomiting)
- Injectable administration (though oral formulations are becoming available)
- Higher cost
Clinical Considerations:
GLP-1 receptor agonists are highly effective for patients needing significant HbA1c reduction and weight loss. They are also beneficial for patients with cardiovascular disease due to their proven cardiovascular benefits.
SGLT2 Inhibitors
Mechanism of Action:
SGLT2 inhibitors reduce blood glucose by inhibiting glucose reabsorption in the kidneys, resulting in increased glucose excretion in the urine. They lower HbA1c by 0.5-1%.
Advantages:
- Weight loss
- Blood pressure reduction
- Cardiovascular and renal benefits (e.g., empagliflozin, canagliflozin)
- Low risk of hypoglycemia
Disadvantages:
- Risk of genitourinary infections
- Potential for volume depletion and hypotension
- Risk of diabetic ketoacidosis
Clinical Considerations:
SGLT2 inhibitors are an excellent choice for patients who need weight loss and cardiovascular or renal protection. However, they should be used cautiously in patients with a history of genitourinary infections or those at risk of dehydration.
Insulin
Mechanism of Action:
Exogenous insulin replaces or supplements endogenous insulin, allowing for precise control of blood glucose levels. The HbA1c reduction is dose-dependent.
Advantages:
- Unlimited potential for HbA1c reduction
- Rapid correction of hyperglycemia
Disadvantages:
- Risk of hypoglycemia
- Weight gain
- Injectable administration
Clinical Considerations:
Insulin therapy is essential for patients with severe hyperglycemia or those who have not achieved glycemic control with other agents. Basal insulin can be added initially, with prandial insulin introduced as needed for further control.
Combining Agents for Optimal Control
Combining different classes of medications can leverage their complementary mechanisms of action, resulting in more effective glycemic control. The choice of combination therapy should be tailored to the patient’s specific needs, considering efficacy, side effects, and comorbidities.
Metformin and Sulfonylurea:
This combination is cost-effective and provides significant HbA1c reduction. However, the risk of hypoglycemia and weight gain must be managed.
Metformin and DPP-4 Inhibitor:
This combination offers moderate HbA1c reduction with a low risk of hypoglycemia and weight gain. It is suitable for patients with modest glycemic elevation.
Metformin and GLP-1 Receptor Agonist:
This combination is highly effective for reducing HbA1c and promoting weight loss. It is particularly beneficial for patients with obesity and cardiovascular disease.
Metformin and SGLT2 Inhibitor:
This combination provides HbA1c reduction, weight loss, and cardiovascular and renal benefits. It is ideal for patients with cardiovascular or renal comorbidities.
Metformin and Insulin:
This combination allows for flexible and precise control of blood glucose levels. It is necessary for patients with severe hyperglycemia or advanced T2DM.
Emerging Therapies and Future Directions
The landscape of T2DM treatment continues to evolve with the development of new therapeutic agents and combinations. Dual GIP/GLP-1 receptor agonists, such as tirzepatide, have shown promising results in clinical trials, offering substantial HbA1c reduction and weight loss. These agents may provide a new frontier in the management of T2DM.
Additionally, research into the pathophysiology of T2DM and the identification of novel therapeutic targets may lead to the development of more effective and personalized treatments. The integration of digital health tools and continuous glucose monitoring (CGM) systems can also enhance the management of T2DM by providing real-time data and enabling more precise adjustments to therapy.
See also: What Does The Pancreas Do In Type 2 Diabetes
Conclusion
Metformin remains a cornerstone of T2DM treatment, but many patients will require additional agents to achieve and maintain glycemic control. The selection of an appropriate add-on therapy should be individualized based on the patient’s characteristics, preferences, and comorbidities. Combining different classes of medications can provide synergistic benefits and improve overall outcomes. As the field of diabetes treatment continues to advance, emerging therapies and innovative approaches hold the promise of further enhancing the management of T2DM and improving the quality of life for patients.
Related topics:
What’s the Most Popular Medication for Type 2 Diabetes