Hypoglycemia, commonly known as low blood sugar, is a condition that can cause a range of symptoms, from mild discomfort to severe health issues. For those who experience hypoglycemia frequently, understanding the root causes is crucial to managing and preventing these episodes. This article delves into the various factors that can make individuals more susceptible to hypoglycemia, exploring the intricate balance of glucose regulation and the potential disturbances that can lead to recurrent low blood sugar levels.
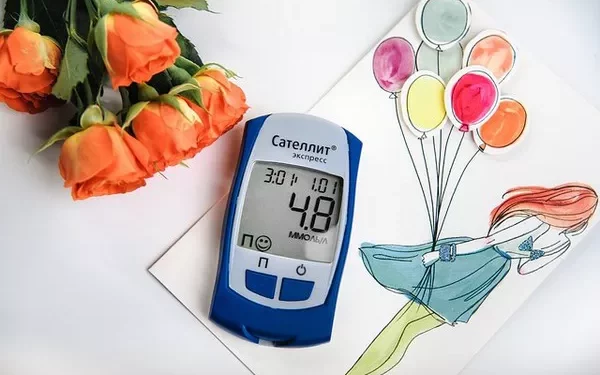
Hypoglycemia occurs when blood glucose levels fall below the normal range, typically below 70 mg/dL (3.9 mmol/L). This condition is particularly concerning for individuals with diabetes who manage their blood sugar through medication or insulin. However, hypoglycemia can also affect non-diabetic individuals, often due to different underlying health issues or lifestyle factors. To understand why some people experience hypoglycemia more easily than others, it is essential to examine the physiological mechanisms of glucose regulation, the role of insulin, and the potential disturbances that can predispose someone to frequent low blood sugar episodes.
The Physiology of Glucose Regulation
The Role of Glucose in the Body
Glucose is a primary energy source for the body’s cells, particularly for the brain, which relies almost exclusively on glucose for its energy needs. The regulation of blood glucose levels is a complex process involving multiple organs, hormones, and metabolic pathways. After consuming carbohydrates, they are broken down into glucose and absorbed into the bloodstream. The pancreas then releases insulin, a hormone that facilitates the uptake of glucose by cells, thus lowering blood glucose levels.
Insulin and Glucagon: The Balancing Act
Insulin and glucagon are the two main hormones involved in maintaining glucose homeostasis. Insulin lowers blood glucose levels by promoting the storage of glucose in the liver and muscle cells as glycogen, while glucagon raises blood glucose levels by stimulating the conversion of glycogen back into glucose. This delicate balance ensures that the body has a steady supply of glucose to meet its energy demands.
Counterregulatory Hormones
In addition to insulin and glucagon, other hormones, known as counterregulatory hormones, play a role in preventing hypoglycemia. These include epinephrine (adrenaline), cortisol, and growth hormone. When blood glucose levels drop, these hormones work to increase glucose production and reduce glucose utilization, thereby raising blood sugar levels. Any disruption in the secretion or action of these hormones can predispose an individual to hypoglycemia.
Common Causes of Hypoglycemia
Diabetes Management
For individuals with diabetes, hypoglycemia is often a side effect of insulin therapy or other glucose-lowering medications. Factors such as incorrect dosage, timing of medication, missed meals, or increased physical activity can disrupt the balance of insulin and glucose, leading to hypoglycemia.
Medication-Induced Hypoglycemia
Apart from diabetes medications, other drugs can also cause hypoglycemia. These include certain antibiotics (like quinolones), antimalarial drugs, and medications for heart conditions. It is important for individuals to be aware of the potential hypoglycemic effects of any medication they are taking and to monitor their blood sugar levels accordingly.
Hormonal Imbalances
Hormonal imbalances can significantly affect glucose regulation. For example, adrenal insufficiency (Addison’s disease) results in low levels of cortisol, which can impair the body’s ability to respond to low blood sugar. Similarly, hypopituitarism, which leads to deficiencies in pituitary hormones, can also predispose individuals to hypoglycemia.
Insulinomas and Other Tumors
Insulinomas are rare tumors of the pancreas that produce excessive amounts of insulin, leading to chronic hypoglycemia. Other types of tumors, such as non-islet cell tumors, can also cause hypoglycemia by producing insulin-like substances or by consuming large amounts of glucose themselves.
Liver Diseases
The liver plays a crucial role in glucose storage and production. Liver diseases, such as hepatitis, cirrhosis, or liver cancer, can impair the liver’s ability to store and release glucose, resulting in hypoglycemia.
Renal Failure
Chronic kidney disease can affect glucose metabolism and the clearance of insulin, leading to an increased risk of hypoglycemia. Additionally, kidney failure can impair the production of glucose from non-carbohydrate sources, further contributing to low blood sugar levels.
Gastrointestinal Surgery
Surgical procedures involving the stomach or intestines, such as gastric bypass surgery, can lead to dumping syndrome, where food moves too quickly from the stomach to the intestines. This can cause rapid spikes and subsequent drops in blood glucose levels, resulting in hypoglycemia.
Lifestyle Factors Contributing to Hypoglycemia
Diet and Nutrition
Diet plays a pivotal role in glucose regulation. Skipping meals, prolonged fasting, or consuming meals that are high in simple sugars but low in complex carbohydrates can cause fluctuations in blood glucose levels. A diet lacking in balanced nutrition can predispose individuals to hypoglycemia, especially if their bodies are unable to store or produce sufficient glucose.
Physical Activity
Exercise increases glucose uptake by muscle cells, which can lead to hypoglycemia if not managed properly. This is particularly true for individuals who engage in prolonged or intense physical activity without adjusting their carbohydrate intake or medication dosage accordingly.
Alcohol Consumption
Alcohol can interfere with the liver’s ability to produce glucose, especially when consumed on an empty stomach or in large quantities. This can lead to delayed hypoglycemia, which may occur several hours after drinking.
Stress and Mental Health
Stress and mental health conditions, such as anxiety and depression, can affect hormone levels and glucose metabolism. Stress triggers the release of counterregulatory hormones, but chronic stress can lead to dysregulation of this response, increasing the risk of hypoglycemia.
Hypoglycemia in Non-Diabetic Individuals
Reactive Hypoglycemia
Reactive hypoglycemia, also known as postprandial hypoglycemia, occurs within a few hours after eating. It is often due to an exaggerated insulin response to a meal. This condition is more common in individuals with prediabetes or those who have had gastric surgery.
Fasting Hypoglycemia
Fasting hypoglycemia occurs when blood glucose levels drop after periods of not eating. This can happen in individuals with metabolic disorders, hormonal deficiencies, or those who consume inadequate calories.
Idiopathic Hypoglycemia
Idiopathic hypoglycemia refers to low blood sugar levels without a known cause. This diagnosis is made after ruling out other potential causes and can be challenging to manage due to the lack of a clear underlying issue.
Diagnostic Approaches to Hypoglycemia
Medical History and Physical Examination
A thorough medical history and physical examination are the first steps in diagnosing the cause of hypoglycemia. This includes reviewing dietary habits, medication use, family history, and any recent illnesses or stressors.
Blood Tests
Blood tests are essential for measuring blood glucose levels and identifying potential causes of hypoglycemia. These tests may include fasting blood glucose, oral glucose tolerance tests, and measurements of insulin, C-peptide, and counterregulatory hormones.
Imaging Studies
In cases where tumors are suspected, imaging studies such as CT scans, MRI, or ultrasound may be necessary to identify insulinomas or other tumors that could be causing hypoglycemia.
Continuous Glucose Monitoring
Continuous glucose monitoring (CGM) devices provide real-time tracking of blood glucose levels, helping to identify patterns and triggers of hypoglycemia. This can be particularly useful for individuals who experience frequent or unpredictable hypoglycemic episodes.
Treatment and Management Strategies
Immediate Treatment
Immediate treatment of hypoglycemia involves consuming fast-acting carbohydrates, such as glucose tablets, juice, or candy. This rapidly raises blood glucose levels and alleviates symptoms. For severe cases, where the individual is unable to consume oral carbohydrates, glucagon injections or intravenous glucose may be necessary.
Long-Term Management
Long-term management of hypoglycemia focuses on addressing the underlying causes and preventing future episodes. This may include adjusting diabetes medications, dietary modifications, lifestyle changes, and treating any underlying health conditions.
Dietary Modifications
Dietary modifications are crucial for managing hypoglycemia. Eating small, frequent meals that include complex carbohydrates, protein, and healthy fats can help maintain stable blood glucose levels. Avoiding high-sugar foods and beverages that cause rapid spikes and drops in blood sugar is also important.
Medication Adjustments
For individuals with diabetes, adjusting the dosage and timing of insulin or other glucose-lowering medications can help prevent hypoglycemia. This should be done in consultation with a healthcare provider to ensure optimal blood glucose control.
Addressing Hormonal Imbalances
Treating hormonal imbalances, such as adrenal insufficiency or thyroid disorders, is essential for preventing hypoglycemia. This may involve hormone replacement therapy or other targeted treatments.
Managing Physical Activity
Proper management of physical activity is important for preventing exercise-induced hypoglycemia. This includes monitoring blood glucose levels before, during, and after exercise, and consuming adequate carbohydrates to match the increased energy expenditure.
Education and Support
Education and support are vital components of hypoglycemia management. Individuals should be educated about the signs and symptoms of hypoglycemia, how to treat it, and how to prevent future episodes. Support from healthcare providers, diabetes educators, and support groups can also be beneficial.
See also: Does Too Much Insulin Cause Hypoglycemia?
Conclusion
Frequent hypoglycemia can significantly impact an individual’s quality of life and overall health. Understanding the various factors that contribute to hypoglycemia is crucial for effective management and prevention. By addressing the underlying causes, making appropriate lifestyle adjustments, and working closely with healthcare providers, individuals can better manage their blood glucose levels and reduce the frequency of hypoglycemic episodes. Ongoing research and advances in glucose monitoring and treatment options continue to improve the outlook for those affected by hypoglycemia, offering hope for a better quality of life and optimal blood glucose control.
Related topics:
Why Does Alcohol Cause Hypoglycemia