Type 1 diabetes (T1D) is a chronic autoimmune disorder characterized by the destruction of insulin-producing beta cells in the pancreas, leading to absolute insulin deficiency. This condition typically manifests in childhood or early adulthood, although it can occur at any age. Unlike type 2 diabetes, which is primarily associated with insulin resistance, T1D results from the body’s immune system attacking its own pancreatic cells, thereby impairing the production of insulin—a hormone crucial for regulating blood sugar levels.
Epidemiology and Pathophysiology
T1D accounts for approximately 5-10% of all diabetes cases worldwide, with variations in incidence across different populations. Genetic predisposition plays a significant role, as individuals with specific human leukocyte antigen (HLA) genotypes are more susceptible to developing T1D. Environmental factors, such as viral infections and dietary factors, may trigger autoimmune responses in genetically predisposed individuals, accelerating the onset of the disease.
The pathophysiology of T1D involves a complex interplay of genetic, immunologic, and environmental factors. Autoimmune destruction of beta cells in the pancreatic islets leads to reduced or absent insulin secretion. This process is mediated by T lymphocytes and other immune cells targeting beta cell antigens, such as insulin itself or glutamic acid decarboxylase (GAD).
Clinical Presentation and Diagnosis
The clinical presentation of T1D is characterized by hyperglycemia, which results from the inability of the body to utilize glucose effectively in the absence of insulin. Common symptoms include polyuria, polydipsia, weight loss, and fatigue. In severe cases, diabetic ketoacidosis (DKA) may occur, characterized by metabolic acidosis, ketosis, and electrolyte disturbances.
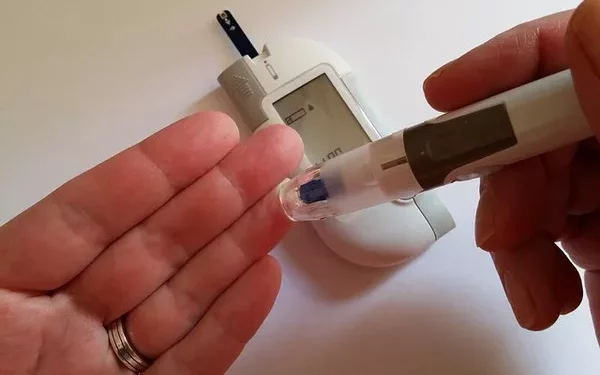
Diagnosis of T1D involves measuring blood glucose levels and assessing glycated hemoglobin (HbA1c) levels. Additional tests such as C-peptide measurement, islet autoantibody testing (e.g., anti-GAD antibodies), and genetic testing may be performed to confirm the autoimmune etiology and distinguish T1D from other forms of diabetes.
Management Strategies
The cornerstone of T1D management is exogenous insulin therapy, which aims to mimic physiological insulin secretion and maintain optimal blood glucose levels. Multiple daily injections of insulin or continuous subcutaneous insulin infusion (insulin pump therapy) are tailored to individual needs based on factors such as diet, physical activity, and insulin sensitivity.
Advanced technologies such as continuous glucose monitoring (CGM) systems and insulin pumps have revolutionized T1D management by providing real-time glucose readings and enabling more precise insulin dosing. Additionally, artificial pancreas systems integrate CGM data with insulin delivery, automating the adjustment of insulin doses to improve glycemic control and reduce the risk of hypoglycemia.
Complications and Long-Term Outcomes
Despite advancements in management, individuals with T1D are at increased risk of developing both acute and chronic complications. Acute complications include hypoglycemia and DKA, which can be life-threatening if not promptly treated. Chronic complications, such as cardiovascular disease, nephropathy, retinopathy, and neuropathy, result from prolonged exposure to hyperglycemia and require comprehensive screening and management to mitigate their impact on health outcomes.
The long-term prognosis of T1D has improved significantly with intensive glycemic control and multidisciplinary care. However, achieving and maintaining target glucose levels remains a challenge, necessitating ongoing education, support, and adjustment of treatment strategies to accommodate individual lifestyles and evolving needs.
Emerging Therapies and Research
Research into T1D focuses on developing strategies to preserve remaining beta cell function, induce immune tolerance, and prevent the onset of the disease in at-risk individuals. Experimental approaches include immunomodulatory therapies, such as antigen-specific immunotherapy and use of monoclonal antibodies targeting immune cells involved in beta cell destruction.
Advancements in stem cell research offer potential avenues for beta cell replacement or regeneration therapies, although significant challenges remain in ensuring long-term efficacy, safety, and practical application in clinical settings.
Psychosocial Considerations and Quality of Life
Living with T1D requires continuous self-management, including monitoring blood glucose levels, calculating insulin doses, and making dietary and lifestyle adjustments. Psychosocial factors, such as diabetes distress and fear of hypoglycemia, significantly impact quality of life and adherence to treatment regimens. Supportive care from healthcare providers, diabetes educators, and peer support networks plays a crucial role in addressing these challenges and promoting holistic well-being.
See also: What Is The Treatment For Type One Diabetes
Conclusion
Type 1 diabetes is a complex autoimmune disorder characterized by insulin deficiency due to beta cell destruction. Its management requires a multidisciplinary approach, encompassing personalized insulin therapy, advanced technologies, and comprehensive care to mitigate acute and chronic complications. Ongoing research into T1D aims to improve treatment outcomes, preserve beta cell function, and enhance quality of life for individuals affected by this challenging condition.
By advancing our understanding of the pathophysiology and optimizing therapeutic strategies, healthcare providers can empower individuals with T1D to achieve better glycemic control, reduce the risk of complications, and lead fulfilling lives despite the demands of lifelong diabetes management.
This article provides a comprehensive overview of T1D, emphasizing its clinical features, management principles, emerging therapies, and the psychosocial impact on affected individuals. Through continued research and collaborative efforts, the medical community strives to improve outcomes and ultimately find a cure for this chronic autoimmune disease.
Related topics:
What Are The 2 Different Types Of Diabetes