Diabetes mellitus, particularly type 2 diabetes, represents a significant health challenge globally, affecting millions of individuals and posing serious risks to long-term health and well-being. As a progressive condition characterized by insulin resistance and relative insulin deficiency, type 2 diabetes requires comprehensive management strategies that encompass medical, lifestyle, and psychological components. This article aims to provide a thorough overview of current practices and recommendations for controlling type 2 diabetes effectively.
Understanding Type 2 Diabetes
Type 2 diabetes accounts for the majority of diabetes cases worldwide. It typically develops in adults but is increasingly seen in younger individuals due to rising obesity rates and sedentary lifestyles. The underlying pathology involves a combination of insulin resistance in peripheral tissues (muscle, liver, and fat) and impaired insulin secretion by pancreatic beta cells. This leads to elevated blood glucose levels (hyperglycemia), which, if left uncontrolled, can contribute to a range of complications affecting the cardiovascular system, kidneys, nerves, and eyes.
Diagnostic Criteria and Monitoring
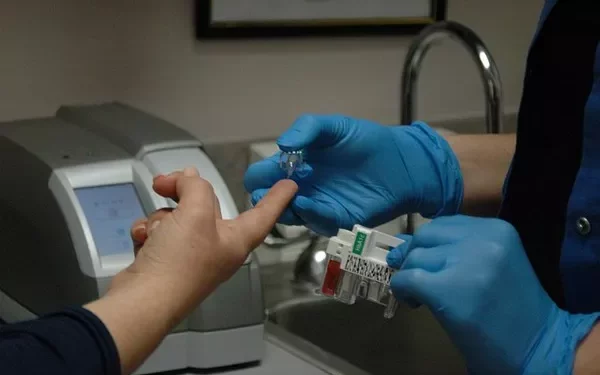
The diagnosis of type 2 diabetes is established through laboratory testing, primarily by measuring fasting plasma glucose, oral glucose tolerance tests, or HbA1c levels. Once diagnosed, regular monitoring of blood glucose levels is crucial to assess treatment efficacy and adjust management strategies accordingly. Additionally, monitoring for complications such as diabetic nephropathy, retinopathy, and cardiovascular disease is essential for comprehensive care.
Medical Management
Pharmacological Interventions
Oral Antidiabetic Agents: The cornerstone of pharmacological management includes various classes of oral medications such as metformin, sulfonylureas, DPP-4 inhibitors, SGLT-2 inhibitors, and GLP-1 receptor agonists. These medications work through different mechanisms to lower blood glucose levels and may be used alone or in combination depending on individual patient needs and response.
Insulin Therapy: Some individuals with type 2 diabetes may require insulin therapy to achieve glycemic control. This can involve basal insulin, prandial insulin, or a combination of both, tailored to the patient’s glucose profile and lifestyle factors. Newer insulin analogs offer improved pharmacokinetic profiles, reducing the risk of hypoglycemia.
Emerging Therapies: Ongoing research continues to explore novel treatments for type 2 diabetes, including dual SGLT-1 and SGLT-2 inhibitors, PPAR agonists, and others targeting specific pathways involved in glucose regulation and insulin sensitivity.
Individualized Treatment Approach
Medical management should be individualized based on factors such as age, comorbidities, diabetes duration, risk of hypoglycemia, patient preferences, and socioeconomic considerations. Regular assessment and adjustment of treatment plans are essential to maintain optimal glycemic control and minimize the risk of complications.
Lifestyle Modifications
Diet and Nutrition
Nutritional Counseling: A balanced diet plays a crucial role in managing type 2 diabetes. Emphasis is placed on carbohydrate counting, portion control, and choosing nutrient-dense foods that promote stable blood glucose levels. Dietary patterns such as the Mediterranean diet or DASH (Dietary Approaches to Stop Hypertension) diet have shown benefits in improving glycemic control and cardiovascular health.
Weight Management: Achieving and maintaining a healthy weight through calorie restriction and regular physical activity is fundamental in diabetes management. Weight loss improves insulin sensitivity and reduces the need for pharmacological interventions in many cases.
Physical Activity
Exercise Recommendations: Regular physical activity, including aerobic exercise, resistance training, and flexibility exercises, helps lower blood glucose levels, improves cardiovascular fitness, and enhances overall well-being. Recommendations include at least 150 minutes per week of moderate-intensity aerobic activity spread over at least three days, with additional muscle-strengthening activities on two or more days per week.
Monitoring During Exercise: Patients should monitor blood glucose levels before, during, and after exercise to prevent hypoglycemia and adjust insulin or carbohydrate intake as needed.
Smoking Cessation and Alcohol Consumption
Smoking: Smoking exacerbates insulin resistance and increases the risk of cardiovascular disease. Smoking cessation is strongly advised as part of diabetes management to reduce these risks.
Alcohol: Moderate alcohol consumption may be permissible but should be done in moderation and with consideration of its potential impact on blood glucose levels and overall health.
Psychosocial Support
Living with type 2 diabetes can be challenging both physically and emotionally. Psychosocial support, including diabetes education, counseling, and support groups, plays a critical role in helping patients cope with the demands of self-management. Addressing psychosocial factors such as stress, depression, and diabetes-related distress can improve treatment adherence and overall quality of life.
Monitoring and Complications Prevention
Regular follow-up visits with healthcare providers are essential to monitor glycemic control, assess for complications, and adjust treatment plans as needed. Screening for diabetic retinopathy, nephropathy, neuropathy, and cardiovascular disease should be conducted regularly to detect and manage complications early.
See also: What Is The Best Oral Diabetes Medication?
Conclusion
Type 2 diabetes management requires a comprehensive, multidisciplinary approach that addresses medical, lifestyle, and psychosocial factors. By focusing on individualized treatment plans, promoting healthy lifestyle modifications, and providing ongoing support and education, healthcare providers can empower patients to effectively control their diabetes and reduce the risk of long-term complications. Continued research and advancements in diabetes care are essential to further improve outcomes and quality of life for individuals living with type 2 diabetes.
In summary, effective management of type 2 diabetes involves a proactive partnership between healthcare providers and patients, emphasizing personalized care, continuous monitoring, and a commitment to lifelong health and well-being. By implementing evidence-based strategies and embracing a holistic approach to diabetes care, we can strive towards better outcomes and improved quality of life for individuals affected by this chronic condition.
Related topics:
What Is The Best Diabetes Type 2 Medication