Hyperglycemia, or elevated blood glucose levels, is a complex and multifaceted phenomenon frequently observed in patients experiencing shock. Shock, a critical condition characterized by inadequate tissue perfusion and oxygenation, can arise from various etiologies such as septic shock, cardiogenic shock, hemorrhagic shock, and anaphylactic shock. The physiological stress associated with shock triggers a cascade of metabolic and hormonal responses that often result in hyperglycemia. This article delves into the underlying mechanisms, clinical implications, and management strategies of hyperglycemia in the context of shock.
Mechanisms Leading to Hyperglycemia in Shock
Stress Response and Counter-Regulatory Hormones
One of the primary drivers of hyperglycemia in shock is the body’s acute stress response. When an individual undergoes shock, the body perceives it as a life-threatening event, prompting the activation of the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system. This activation leads to the release of stress hormones such as cortisol, catecholamines (epinephrine and norepinephrine), glucagon, and growth hormone.
- Cortisol: This glucocorticoid hormone is released from the adrenal cortex in response to adrenocorticotropic hormone (ACTH) from the pituitary gland. Cortisol promotes gluconeogenesis, the process by which glucose is synthesized from non-carbohydrate substrates such as amino acids and glycerol. It also inhibits insulin secretion and impairs peripheral glucose uptake, contributing to increased blood glucose levels.
- Catecholamines: Epinephrine and norepinephrine are potent stimulators of glycogenolysis (the breakdown of glycogen to glucose) in the liver and muscle tissues. They also inhibit insulin release from the pancreas and promote lipolysis, which increases free fatty acid levels and further supports gluconeogenesis.
- Glucagon: Secreted by the alpha cells of the pancreas, glucagon enhances glycogenolysis and gluconeogenesis. In shock, glucagon levels rise significantly, amplifying hyperglycemia.
- Growth Hormone: Released from the pituitary gland, growth hormone antagonizes insulin action, reduces glucose uptake in muscles, and increases lipolysis, contributing to elevated blood glucose levels.
Inflammatory Response and Cytokines
Shock, particularly septic shock, triggers a robust inflammatory response characterized by the release of pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α), interleukins (IL-1, IL-6), and interferon-gamma (IFN-γ). These cytokines play a crucial role in the development of hyperglycemia through several mechanisms:
- Insulin Resistance: Inflammatory cytokines interfere with insulin signaling pathways, leading to decreased insulin sensitivity in peripheral tissues. This insulin resistance results in reduced glucose uptake by muscle and adipose tissues, contributing to elevated blood glucose levels.
- Endothelial Dysfunction: Cytokines can cause endothelial cell damage and dysfunction, impairing insulin-mediated glucose transport across the endothelial barrier.
- Direct Hepatic Effects: Cytokines stimulate hepatic gluconeogenesis and glycogenolysis, further increasing glucose production.
Impaired Insulin Secretion and Action
The pancreatic beta cells’ ability to secrete insulin can be compromised in shock due to direct effects of cytokines and stress hormones, as well as ischemia and hypoxia. Additionally, stress hormones and inflammatory mediators impair insulin signaling pathways, reducing insulin’s efficacy in promoting glucose uptake and utilization.
Clinical Implications of Hyperglycemia in Shock
Hyperglycemia in shock is not merely a biochemical anomaly but has significant clinical implications that can influence patient outcomes.
Impaired Immune Function
Chronic hyperglycemia is known to impair immune function, increasing susceptibility to infections. In the context of shock, acute hyperglycemia can exacerbate immune dysfunction, complicating the clinical course of septic shock and increasing the risk of secondary infections.
Increased Mortality and Morbidity
Numerous studies have demonstrated a correlation between hyperglycemia and increased mortality in critically ill patients, including those with shock. Hyperglycemia can exacerbate the underlying pathophysiology of shock, such as endothelial dysfunction, pro-thrombotic state, and impaired microcirculation, leading to worsened outcomes.
Organ Dysfunction
Hyperglycemia can contribute to organ dysfunction in shock through several mechanisms:
- Cardiovascular System: Hyperglycemia-induced oxidative stress and endothelial dysfunction can impair myocardial function and contribute to arrhythmias, increasing the risk of cardiogenic shock.
- Renal System: Acute kidney injury is a common complication of shock, and hyperglycemia can exacerbate renal damage by promoting glomerular hyperfiltration, increased renal oxygen demand, and tubular injury.
- Neurological System: Hyperglycemia can exacerbate cerebral ischemia and increase the risk of neurological complications such as encephalopathy and seizures in patients with shock.
Delayed Wound Healing
In patients with traumatic injuries or surgical wounds, hyperglycemia can impair wound healing by affecting collagen synthesis, fibroblast proliferation, and angiogenesis. This can lead to increased wound infections and delayed recovery in patients with hemorrhagic or traumatic shock.
Management of Hyperglycemia in Shock
Effective management of hyperglycemia in shock involves a multifaceted approach that includes optimizing glycemic control, addressing the underlying cause of shock, and mitigating the adverse effects of hyperglycemia.
Glycemic Control
The management of hyperglycemia in critically ill patients, including those in shock, requires careful consideration of target glucose levels and appropriate therapeutic interventions.
- Insulin Therapy: Intravenous insulin infusion is the mainstay of treatment for hyperglycemia in critically ill patients. Tight glycemic control (maintaining blood glucose levels between 140-180 mg/dL) is recommended to avoid the detrimental effects of both hyperglycemia and hypoglycemia. Continuous glucose monitoring and frequent adjustments of insulin dosing are essential to achieve optimal glycemic control.
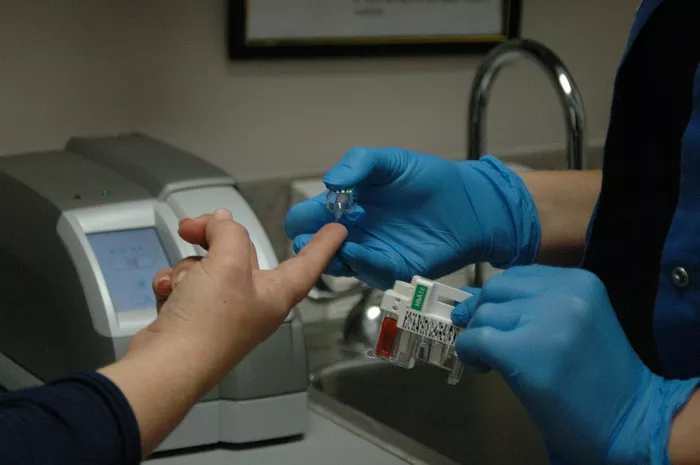
- Glucose Monitoring: Regular monitoring of blood glucose levels is crucial for patients in shock. Point-of-care glucose testing and continuous glucose monitoring systems can provide real-time data to guide insulin therapy and prevent extreme fluctuations in blood glucose levels.
Addressing Underlying Cause
Successful management of hyperglycemia in shock necessitates addressing the underlying cause of shock. This includes:
- Source Control in Sepsis: In septic shock, early identification and control of the infection source (e.g., surgical debridement, drainage of abscesses, removal of infected devices) are critical.
- Fluid Resuscitation: Adequate fluid resuscitation is essential to restore intravascular volume and improve tissue perfusion. Crystalloids, colloids, and blood products may be used based on the type and severity of shock.
- Vasoactive Agents: In patients with refractory hypotension despite adequate fluid resuscitation, vasoactive agents such as norepinephrine, vasopressin, and epinephrine may be necessary to maintain adequate mean arterial pressure and perfusion.
- Oxygenation and Ventilation: Ensuring adequate oxygenation and ventilation is vital, particularly in patients with septic shock or acute respiratory distress syndrome (ARDS). Mechanical ventilation and supplemental oxygen may be required.
Mitigating Adverse Effects
Minimizing the adverse effects of hyperglycemia involves a combination of pharmacological and non-pharmacological strategies.
- Antioxidant Therapy: Antioxidants such as vitamin C and E have been studied for their potential to reduce oxidative stress and endothelial damage associated with hyperglycemia. However, their routine use in critically ill patients remains controversial and requires further investigation.
- Anti-inflammatory Agents: Modulating the inflammatory response in shock may help mitigate the effects of hyperglycemia. Corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs), and newer anti-inflammatory agents are being explored for their potential benefits.
- Nutritional Support: Adequate nutritional support is essential to prevent catabolism and support recovery in patients with shock. Enteral nutrition is preferred over parenteral nutrition, as it preserves gut integrity and reduces the risk of infections. Managing carbohydrate intake and avoiding excessive glucose infusion are important to prevent exacerbation of hyperglycemia.
Conclusion
Hyperglycemia in shock is a complex interplay of hormonal, metabolic, and inflammatory responses. Understanding the underlying mechanisms and clinical implications of hyperglycemia in shock is crucial for effective management and improving patient outcomes. Tight glycemic control, addressing the underlying cause of shock, and mitigating the adverse effects of hyperglycemia are essential components of the therapeutic approach. Ongoing research and clinical trials continue to enhance our understanding of hyperglycemia in critically ill patients and refine management strategies to optimize care in this challenging patient population.
Related topics:
How Does Pancreatitis Cause Hyperglycemia?