Hyperglycemia, a condition characterized by elevated blood glucose levels, is a significant health concern, particularly for individuals with diabetes. It is imperative for healthcare professionals, patients, and caregivers to understand the nuances of hyperglycemia to manage it effectively and prevent its complications. This article delves into the critical aspects of hyperglycemia, including its definition, causes, symptoms, diagnosis, and management strategies.
Defining Hyperglycemia
Hyperglycemia occurs when there is an excessive amount of glucose in the blood. According to the American Diabetes Association (ADA), hyperglycemia is typically defined as a blood glucose level higher than 180 mg/dL (10.0 mmol/L) after a meal or higher than 130 mg/dL (7.2 mmol/L) in a fasting state. These thresholds are crucial for identifying and managing hyperglycemia effectively.
Causes of Hyperglycemia
Hyperglycemia can result from various factors, often related to insufficient insulin production or action. Understanding these causes is vital for both prevention and treatment.
1. Insufficient Insulin Production
Type 1 diabetes is characterized by an autoimmune response that destroys insulin-producing beta cells in the pancreas. Without adequate insulin, glucose cannot enter the cells, leading to elevated blood sugar levels.
2. Insulin Resistance
In Type 2 diabetes, the body’s cells become resistant to insulin, meaning they do not respond appropriately to the hormone. As a result, glucose accumulates in the bloodstream.
3. Dietary Factors
Consuming excessive carbohydrates, especially simple sugars, can lead to spikes in blood glucose levels. Poor meal planning and overeating contribute significantly to hyperglycemia.
4. Physical Inactivity
Regular physical activity helps regulate blood sugar levels by increasing insulin sensitivity. A sedentary lifestyle can exacerbate insulin resistance and elevate glucose levels.
5. Stress
Both physical and emotional stress can trigger the release of hormones such as cortisol and adrenaline, which increase blood sugar levels.
6. Illness and Infection
During illness or infection, the body’s stress response can increase blood glucose levels. Additionally, certain medications used to treat infections or other conditions can also contribute to hyperglycemia.
Symptoms of Hyperglycemia
Recognizing the symptoms of hyperglycemia is crucial for timely intervention. Common symptoms include:
- Increased thirst and dry mouth
- Frequent urination
- Fatigue and weakness
- Blurred vision
- Headache
- Difficulty concentrating
In severe cases, hyperglycemia can lead to diabetic ketoacidosis (DKA) in Type 1 diabetes or hyperosmolar hyperglycemic state (HHS) in Type 2 diabetes, both of which require emergency medical attention.
Diagnosis of Hyperglycemia
Diagnosing hyperglycemia involves measuring blood glucose levels using various methods. These include:
1. Fasting Blood Glucose Test
This test measures blood glucose levels after an overnight fast. A level of 126 mg/dL (7.0 mmol/L) or higher on two separate occasions indicates diabetes.
2. Oral Glucose Tolerance Test (OGTT)
In this test, blood glucose levels are measured before and after consuming a sugary drink. A level of 200 mg/dL (11.1 mmol/L) or higher two hours after ingestion indicates diabetes.
3. Random Blood Glucose Test
A blood glucose level of 200 mg/dL (11.1 mmol/L) or higher at any time of day, along with symptoms of hyperglycemia, can indicate diabetes.
4. Hemoglobin A1c Test
The A1c test measures the average blood glucose levels over the past two to three months. An A1c level of 6.5% or higher on two separate occasions confirms a diabetes diagnosis.
Managing Hyperglycemia
Effective management of hyperglycemia involves a multifaceted approach that includes medication, lifestyle changes, and regular monitoring.
1. Medication
Medications for managing hyperglycemia vary depending on the type of diabetes and the individual’s health status. These include:
a. Insulin Therapy
Insulin is essential for individuals with Type 1 diabetes and for some with Type 2 diabetes. Different types of insulin (rapid-acting, short-acting, intermediate-acting, and long-acting) are used to mimic the body’s natural insulin patterns.
b. Oral Hypoglycemic Agents
Several oral medications help lower blood glucose levels in people with Type 2 diabetes. These include metformin, sulfonylureas, meglitinides, thiazolidinediones, DPP-4 inhibitors, and SGLT2 inhibitors.
c. GLP-1 Receptor Agonists
These injectable medications help lower blood sugar by increasing insulin secretion, decreasing glucagon secretion, and slowing gastric emptying.
2. Lifestyle Changes
Lifestyle modifications play a crucial role in managing hyperglycemia. These include:
a. Healthy Eating
A balanced diet that includes complex carbohydrates, fiber, lean proteins, and healthy fats helps maintain stable blood glucose levels. The ADA recommends carbohydrate counting, portion control, and meal planning as effective strategies.
b. Regular Physical Activity
Engaging in regular exercise, such as walking, swimming, or cycling, improves insulin sensitivity and helps lower blood glucose levels. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, along with strength training exercises.
c. Weight Management
Maintaining a healthy weight is essential for managing hyperglycemia, particularly in individuals with Type 2 diabetes. Even modest weight loss can improve blood glucose control.
3. Monitoring Blood Glucose Levels
Regular monitoring of blood glucose levels is vital for individuals with diabetes. This helps track the effectiveness of treatment and make necessary adjustments. Monitoring methods include:
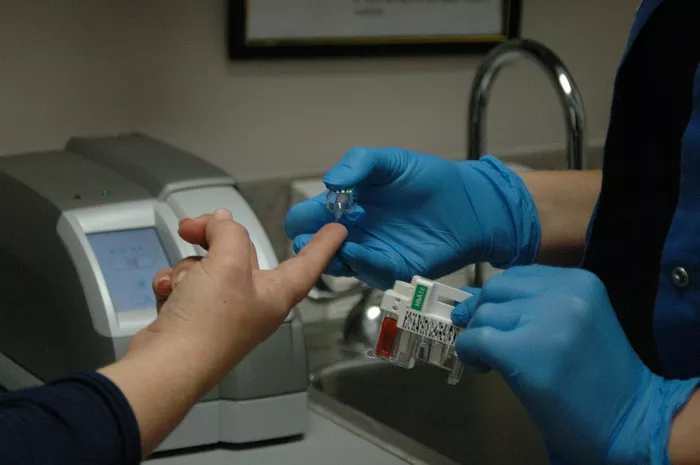
a. Self-Monitoring of Blood Glucose (SMBG)
Using a blood glucose meter to check levels at home provides immediate feedback. The frequency of testing varies based on individual treatment plans and type of diabetes.
b. Continuous Glucose Monitoring (CGM)
CGM devices provide real-time glucose readings throughout the day and night. They help identify patterns and trends, allowing for more precise adjustments to treatment.
4. Managing Stress
Stress management techniques, such as mindfulness meditation, deep breathing exercises, and yoga, can help reduce stress-related spikes in blood glucose levels.
Complications of Untreated Hyperglycemia
Untreated or poorly managed hyperglycemia can lead to serious complications, both acute and chronic.
1. Acute Complications
a. Diabetic Ketoacidosis (DKA)
DKA is a life-threatening condition that occurs primarily in individuals with Type 1 diabetes. It results from a severe lack of insulin, leading to the breakdown of fats and the production of ketones, which cause the blood to become acidic. Symptoms include nausea, vomiting, abdominal pain, and altered mental status. Immediate medical attention is required.
b. Hyperosmolar Hyperglycemic State (HHS)
HHS is a severe complication seen in Type 2 diabetes, characterized by extremely high blood glucose levels and severe dehydration. It often develops over days or weeks and can lead to seizures, coma, or death if not treated promptly.
2. Chronic Complications
a. Cardiovascular Disease
Persistent hyperglycemia increases the risk of cardiovascular diseases, including coronary artery disease, stroke, and peripheral artery disease.
b. Neuropathy
High blood sugar levels can damage nerves throughout the body, leading to diabetic neuropathy. This condition can cause pain, tingling, and loss of sensation, particularly in the extremities.
c. Nephropathy
Diabetic nephropathy, or kidney disease, results from damage to the blood vessels in the kidneys. This can lead to kidney failure and the need for dialysis or transplantation.
d. Retinopathy
Diabetic retinopathy is a leading cause of blindness in adults. It occurs when high blood sugar levels damage the blood vessels in the retina.
e. Foot Complications
Nerve damage and poor circulation resulting from hyperglycemia can lead to foot ulcers and infections. Severe cases may require amputation.
Preventing Hyperglycemia
Prevention strategies for hyperglycemia focus on maintaining stable blood glucose levels through a combination of medication, lifestyle changes, and regular monitoring.
1. Adherence to Medication
Taking prescribed medications as directed by a healthcare provider is crucial for managing blood glucose levels and preventing hyperglycemia.
2. Healthy Eating Habits
Consuming a balanced diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats helps maintain stable blood glucose levels. Avoiding sugary beverages and processed foods is also important.
3. Regular Exercise
Incorporating regular physical activity into daily routines helps improve insulin sensitivity and lower blood glucose levels.
4. Weight Management
Achieving and maintaining a healthy weight can significantly reduce the risk of hyperglycemia and its associated complications.
5. Routine Monitoring
Regularly monitoring blood glucose levels helps detect early signs of hyperglycemia and allows for timely intervention.
6. Stress Management
Practicing stress-reducing techniques, such as meditation, yoga, and deep breathing exercises, can help prevent stress-induced spikes in blood glucose levels.
Conclusion
Hyperglycemia, characterized by elevated blood glucose levels, poses significant health risks, particularly for individuals with diabetes. Understanding its causes, symptoms, and management strategies is essential for preventing and treating this condition effectively. Through a combination of medication, lifestyle changes, and regular monitoring, individuals can maintain stable blood glucose levels and reduce the risk of complications associated with hyperglycemia. As healthcare professionals, it is our responsibility to educate and support patients in their journey to manage their blood sugar levels and lead healthier lives.
Related topics:
Stress Induced Hyperglycemia In Non Diabetics