Introduction
Hypoglycemia and hyperglycemia are two critical conditions associated with the regulation of blood glucose levels in the body, primarily concerning individuals with diabetes. Understanding the relationship between these conditions is crucial for effective diabetes management and prevention of complications. This article delves into the mechanisms by which hypoglycemia can induce hyperglycemia, exploring the physiological responses and implications for diabetic patients.
Understanding Hypoglycemia and Hyperglycemia
Hypoglycemia occurs when blood glucose levels drop below the normal range, typically less than 70 mg/dL. It can manifest through symptoms such as shakiness, sweating, confusion, and in severe cases, loss of consciousness. On the other hand, hyperglycemia refers to elevated blood glucose levels, often exceeding 180 mg/dL after meals and 130 mg/dL in a fasting state. Chronic hyperglycemia is a hallmark of diabetes and can lead to serious complications, including cardiovascular disease, neuropathy, retinopathy, and nephropathy.
Mechanisms Linking Hypoglycemia to Hyperglycemia
1. Counterregulatory Hormone Response
When blood glucose levels fall too low, the body initiates a counterregulatory response to restore normoglycemia. This involves the release of several hormones, including glucagon, epinephrine, norepinephrine, cortisol, and growth hormone. These hormones work collectively to increase blood glucose levels through various mechanisms:
- Glucagon: Secreted by the alpha cells of the pancreas, glucagon promotes glycogenolysis (the breakdown of glycogen into glucose) and gluconeogenesis (the production of glucose from non-carbohydrate substrates) in the liver.
- Epinephrine and Norepinephrine: Released from the adrenal medulla, these catecholamines stimulate glycogenolysis and inhibit insulin secretion, thereby increasing blood glucose.
- Cortisol: A glucocorticoid hormone from the adrenal cortex, cortisol enhances gluconeogenesis and decreases glucose uptake in tissues.
- Growth Hormone: Released from the pituitary gland, growth hormone decreases glucose uptake in tissues and promotes lipolysis, indirectly raising blood glucose levels.
The combined effect of these hormones is to rapidly elevate blood glucose, preventing prolonged hypoglycemia. However, in some instances, this counterregulatory response can overshoot, leading to subsequent hyperglycemia.
2. The Somogyi Effect
The Somogyi effect, also known as rebound hyperglycemia, is a phenomenon where an episode of untreated nighttime hypoglycemia leads to high blood glucose levels in the morning. This occurs as a result of the counterregulatory hormone response described above. Patients may experience nocturnal hypoglycemia due to excessive insulin doses or missed meals. During sleep, the body compensates for the low glucose levels by releasing counterregulatory hormones, resulting in hyperglycemia upon waking.
3. Reactive Hyperglycemia
Reactive hyperglycemia is another condition where blood glucose levels rise significantly after a hypoglycemic episode. This is often observed after consuming a carbohydrate-rich meal following hypoglycemia. The body’s sensitivity to insulin can be temporarily diminished due to the prior counterregulatory hormone surge, causing a larger-than-normal glucose spike postprandially.
4. Hypoglycemia-Associated Autonomic Failure (HAAF)
Frequent hypoglycemic episodes can lead to a condition known as hypoglycemia-associated autonomic failure (HAAF). This is characterized by a blunted counterregulatory hormone response and impaired awareness of hypoglycemia. As a result, the body becomes less efficient at detecting and correcting low blood glucose levels, increasing the risk of severe hypoglycemia and subsequent hyperglycemia due to delayed or exaggerated counterregulatory responses.
5. Stress-Induced Hyperglycemia
Hypoglycemia is a significant stressor for the body, triggering the release of stress hormones like cortisol and catecholamines. These hormones not only contribute to the immediate counterregulatory response but can also have prolonged effects on blood glucose regulation. Chronic stress can lead to sustained hyperglycemia due to increased hepatic glucose production and reduced peripheral glucose uptake.
6. Insulin Resistance
Repeated hypoglycemic events can lead to fluctuations in insulin sensitivity. Initially, hypoglycemia may increase insulin sensitivity, but over time, the body may develop resistance to the hormone due to the frequent activation of counterregulatory mechanisms. This insulin resistance can exacerbate hyperglycemia, making it more challenging to maintain stable blood glucose levels.
7. Behavioral and Lifestyle Factors
The experience of hypoglycemia can influence a patient’s behavior and lifestyle choices. Fear of hypoglycemia may lead patients to reduce their insulin doses or overconsume carbohydrates, both of which can result in hyperglycemia. Additionally, hypoglycemia can impair cognitive function, leading to poor decision-making regarding diabetes management.
8. Impact on Glucose-Sensing Mechanisms
Frequent hypoglycemia can alter the body’s glucose-sensing mechanisms, particularly in the brain. The hypothalamus, which plays a crucial role in regulating energy homeostasis, may become less responsive to low glucose levels. This impaired glucose sensing can disrupt the balance of insulin and counterregulatory hormones, contributing to the development of hyperglycemia.
Clinical Implications
Understanding the interplay between hypoglycemia and hyperglycemia is vital for clinicians managing patients with diabetes. Here are some key considerations:
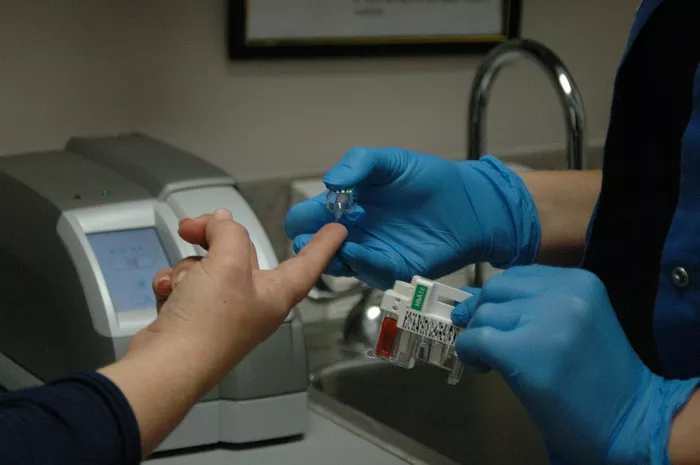
1. Monitoring and Education
Regular monitoring of blood glucose levels is essential to identify patterns of hypoglycemia and hyperglycemia. Continuous glucose monitoring (CGM) systems can provide real-time data, helping patients and healthcare providers to detect and address fluctuations promptly. Education on recognizing symptoms and managing both hypoglycemia and hyperglycemia is crucial for patient empowerment and effective self-management.
2. Individualized Treatment Plans
Diabetes management should be personalized to account for the unique needs and responses of each patient. This includes tailoring insulin regimens, dietary plans, and lifestyle recommendations. Adjusting insulin doses to prevent nighttime hypoglycemia and rebound hyperglycemia is particularly important. Clinicians should also consider the timing and composition of meals to minimize the risk of reactive hyperglycemia.
3. Addressing Hypoglycemia Unawareness
For patients with HAAF, restoring hypoglycemia awareness is a critical goal. This can involve structured education programs, the use of CGM systems, and adjusting glycemic targets to avoid frequent hypoglycemic episodes. Ensuring that patients have a clear plan for managing hypoglycemia, including carrying fast-acting carbohydrates, is essential.
4. Psychological Support
Fear of hypoglycemia can significantly impact a patient’s quality of life and diabetes management. Providing psychological support and counseling can help patients cope with anxiety related to hypoglycemia and encourage adherence to treatment plans. Cognitive-behavioral therapy (CBT) and stress management techniques may be beneficial.
5. Addressing Insulin Resistance
Managing insulin resistance requires a multifaceted approach. This includes optimizing medication regimens, encouraging regular physical activity, and promoting weight management. In some cases, medications that improve insulin sensitivity, such as metformin or thiazolidinediones, may be appropriate.
6. Avoiding Overcorrection
In response to hypoglycemia, patients and caregivers must be cautious not to overcorrect with excessive carbohydrate intake. Educating patients on the appropriate amounts of fast-acting carbohydrates to consume during a hypoglycemic episode can prevent subsequent hyperglycemia. Emphasizing the importance of rechecking blood glucose levels after treatment is also crucial.
Research and Future Directions
Ongoing research continues to explore the complex relationship between hypoglycemia and hyperglycemia. Areas of interest include:
1. Novel Therapies
Developing new therapies that can modulate the counterregulatory hormone response to prevent extreme fluctuations in blood glucose levels is a promising area of research. This includes the use of novel pharmacological agents and advanced insulin formulations.
2. Improved Glucose Monitoring
Advancements in glucose monitoring technology, such as next-generation CGM systems and implantable sensors, are likely to enhance our ability to detect and manage hypoglycemia and hyperglycemia more effectively. These technologies can provide more accurate and continuous data, enabling better clinical decision-making.
3. Understanding Glucose Sensing
Further research into the mechanisms of glucose sensing in the brain and peripheral tissues could lead to new insights and therapeutic targets. Understanding how these mechanisms are altered in diabetes and by frequent hypoglycemic episodes is crucial for developing effective interventions.
4. Behavioral Interventions
Exploring the impact of behavioral interventions, including psychological support and education programs, on the management of hypoglycemia and hyperglycemia is an important area of study. Identifying strategies that can improve patient adherence and reduce fear of hypoglycemia can have a significant impact on diabetes outcomes.
5. Precision Medicine
The application of precision medicine approaches, which tailor treatment based on individual genetic, environmental, and lifestyle factors, has the potential to revolutionize diabetes management. Identifying biomarkers that predict susceptibility to hypoglycemia or hyperglycemia can help personalize treatment plans and improve outcomes.
Conclusion
Hypoglycemia and hyperglycemia are closely interconnected conditions that require careful management in individuals with diabetes. The body’s counterregulatory response to hypoglycemia, while essential for survival, can inadvertently lead to hyperglycemia through various mechanisms. Understanding these processes is crucial for clinicians to develop effective treatment strategies and for patients to manage their condition successfully. Through ongoing research, improved technologies, and personalized care, we can better address the challenges posed by these blood glucose fluctuations and enhance the quality of life for those living with diabetes.
Related topics:
Do Not Eat These Food, If You Have High Blood Sugar
What Should You Eat Immediately If Your Blood Sugar Is High?