In the realm of diabetes management and metabolic health, understanding the nuances between various types of glucose measurements is paramount. Two primary methods utilized for assessing glucose levels are plasma glucose and blood glucose measurements. While these terms may seem interchangeable, they represent distinct aspects of glucose concentration within the body. In this comprehensive article, we delve into the fundamental disparities between plasma glucose and blood glucose, elucidating their physiological underpinnings, measurement techniques, clinical significance, and implications for diabetes care and metabolic health.
1. Understanding Plasma Glucose:
Plasma glucose refers to the concentration of glucose molecules present in the liquid component of blood known as plasma. Plasma is the straw-colored, liquid portion of blood that remains after the cells (red blood cells, white blood cells, and platelets) are removed through centrifugation. Glucose is transported in the bloodstream primarily in the form of plasma, where it serves as a vital energy source for cells throughout the body.
Key Aspects of Plasma Glucose:
- Physiological Distribution: Glucose is absorbed from the gastrointestinal tract into the bloodstream after meals and is transported to various tissues and organs via the circulatory system. In the fasting state, glucose is maintained within a narrow range through a balance of hepatic glucose production, glucose utilization by peripheral tissues, and hormonal regulation.
- Measurement Technique: Plasma glucose levels are typically measured using laboratory-based assays that quantify the concentration of glucose molecules in a plasma sample obtained through venipuncture (phlebotomy). These assays utilize enzymatic reactions or spectrophotometry to determine glucose concentrations in units of milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L).
- Clinical Significance: Plasma glucose levels are a primary determinant in the diagnosis and management of diabetes mellitus and other metabolic disorders. Fasting plasma glucose (FPG) levels, oral glucose tolerance test (OGTT) results, and random plasma glucose measurements are used to diagnose diabetes and assess glycemic control in individuals with diabetes.
2. Understanding Blood Glucose:
Blood glucose, on the other hand, encompasses the concentration of glucose molecules present in the entire blood sample, including both plasma and cellular components. While plasma glucose provides a snapshot of glucose concentration in the liquid portion of blood, blood glucose reflects the total glucose content within the bloodstream, encompassing both plasma and cellular glucose.
Key Aspects of Blood Glucose:
- Comprehensive Assessment: Blood glucose measurements offer a holistic evaluation of glucose concentration within the bloodstream, accounting for both plasma glucose and glucose contained within red blood cells and other cellular elements. This provides a broader perspective on overall glycemic status and metabolic health.
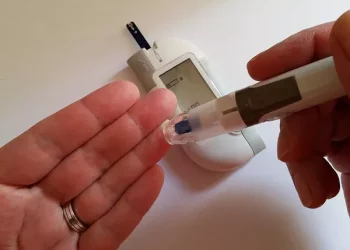
- Measurement Technique: Blood glucose levels can be measured using various methods, including point-of-care testing with handheld glucometers, laboratory-based assays using venous or capillary blood samples, and continuous glucose monitoring (CGM) systems. Glucometers utilize enzymatic reactions to quantify glucose levels in whole blood samples and provide immediate results at the point of care.
- Clinical Significance: Blood glucose measurements are widely used in clinical practice for diabetes management, glucose monitoring during hospitalization, perioperative care, and critical care settings. Continuous glucose monitoring (CGM) systems offer real-time monitoring of interstitial fluid glucose levels and are used to track glucose trends and patterns over time.
3. Key Differences Between Plasma Glucose and Blood Glucose:
While plasma glucose and blood glucose measurements are closely related, they differ in several key aspects:
- Physiological Distribution: Plasma glucose reflects the concentration of glucose molecules in the liquid portion of blood (plasma), whereas blood glucose encompasses the total glucose content within the bloodstream, including both plasma and cellular components.
- Measurement Technique: Plasma glucose levels are measured using laboratory-based assays that quantify glucose concentration in a plasma sample obtained through venipuncture, while blood glucose levels can be measured using handheld glucometers, laboratory-based assays, or continuous glucose monitoring (CGM) systems.
- Clinical Application: Plasma glucose levels are utilized for the diagnosis and management of diabetes mellitus and other metabolic disorders, whereas blood glucose measurements are used for real-time glucose monitoring in various clinical settings, including diabetes management, hospitalization, and critical care.
4. Clinical Utility and Implications:
Both plasma glucose and blood glucose measurements play crucial roles in diabetes management, metabolic health assessment, and clinical decision-making. Plasma glucose levels provide valuable information for diagnosing diabetes, assessing glycemic control, and guiding treatment decisions, while blood glucose measurements offer real-time monitoring capabilities and insights into glucose trends and patterns over time.
5. Conclusion:
In conclusion, while plasma glucose and blood glucose measurements are closely related, they represent distinct aspects of glucose concentration within the bloodstream. Plasma glucose reflects the concentration of glucose molecules in the liquid portion of blood, whereas blood glucose encompasses the total glucose content within the bloodstream, including both plasma and cellular components. By understanding the disparities between plasma glucose and blood glucose measurements and leveraging their complementary information, healthcare providers can effectively assess glycemic control, diagnose diabetes, and optimize treatment regimens for individuals with diabetes and other metabolic disorders.