Type 1 diabetes, often referred to as insulin-dependent diabetes mellitus (IDDM), is a chronic autoimmune condition characterized by the destruction of insulin-producing beta cells in the pancreas. Individuals with type 1 diabetes require lifelong insulin therapy to regulate their blood glucose levels effectively and prevent complications associated with hyperglycemia. While insulin remains the cornerstone of treatment for type 1 diabetes, various adjunctive therapies and management strategies play pivotal roles in optimizing glycemic control, mitigating risks, and enhancing quality of life for individuals with this condition. This article provides a comprehensive overview of the treatment modalities and approaches used in the management of type 1 diabetes.
1. Insulin Therapy: The Foundation of Type 1 Diabetes Management
Insulin therapy serves as the foundation of treatment for individuals with type 1 diabetes, replacing the deficient endogenous insulin production and facilitating glucose uptake by cells throughout the body. Several types of insulin are available, each with distinct onset, peak, and duration of action, allowing for tailored insulin regimens to meet individual needs. These insulin types include:
- Rapid-Acting Insulin Analogues: Rapid-acting insulin analogues, such as insulin lispro (e.g., Humalog), insulin aspart (e.g., NovoLog), and insulin glulisine (e.g., Apidra), have a rapid onset of action, typically within 15 minutes of administration, and are used to cover mealtime insulin needs.
- Short-Acting Insulin: Regular human insulin, also known as short-acting insulin, has a slower onset of action compared to rapid-acting analogues and is typically administered 30 to 45 minutes before meals to cover postprandial glucose excursions.
- Intermediate-Acting Insulin: Intermediate-acting insulins, such as NPH (Neutral Protamine Hagedorn) insulin, have a delayed onset and longer duration of action, providing basal insulin coverage to maintain stable blood glucose levels between meals and overnight.
- Long-Acting Insulin Analogues: Long-acting insulin analogues, such as insulin glargine (e.g., Lantus, Basaglar, Toujeo) and insulin detemir (e.g., Levemir), have a consistent and prolonged duration of action, offering basal insulin coverage for up to 24 hours with once-daily or twice-daily dosing.
Individuals with type 1 diabetes often use a combination of rapid-acting and long-acting insulins in their treatment regimen, known as basal-bolus insulin therapy, to mimic the physiological pattern of insulin secretion and achieve optimal glycemic control.
2. Continuous Glucose Monitoring (CGM) Systems
Continuous glucose monitoring (CGM) systems are valuable tools in the management of type 1 diabetes, providing real-time information about glucose levels and trends throughout the day and night. CGM systems consist of a small sensor inserted under the skin to measure interstitial glucose levels, a transmitter that sends glucose data to a receiver or smartphone app, and alarms/alerts to notify users of hypo- or hyperglycemic events.
CGM systems offer several benefits for individuals with type 1 diabetes, including:
- Improved Glycemic Control: CGM systems enable individuals to monitor their glucose levels continuously and make timely adjustments to insulin doses, diet, and physical activity to maintain stable blood glucose levels.
- Reduced Hypoglycemia: CGM systems provide early detection of hypoglycemic events, allowing individuals to take corrective action promptly and minimize the risk of severe hypoglycemia.
- Enhanced Quality of Life: By providing real-time glucose data and reducing the need for frequent fingerstick blood glucose testing, CGM systems offer convenience, flexibility, and peace of mind for individuals with type 1 diabetes and their caregivers.
Recent advancements in CGM technology, such as integrated insulin pump systems (sensor-augmented pump therapy) and predictive low glucose suspend (PLGS) features, further enhance the capabilities and benefits of CGM for type 1 diabetes management.
3. Insulin Pump Therapy
Insulin pump therapy, also known as continuous subcutaneous insulin infusion (CSII), offers an alternative to multiple daily injections for individuals with type 1 diabetes. Insulin pumps deliver rapid-acting insulin continuously through a small catheter inserted under the skin, providing basal insulin coverage throughout the day and allowing for precise bolus insulin dosing with meals and snacks.
Insulin pump therapy offers several advantages for individuals with type 1 diabetes, including:
- Flexible Insulin Delivery: Insulin pumps allow for personalized basal insulin rates and bolus insulin doses, providing flexibility to accommodate variations in meal patterns, physical activity, and lifestyle factors.
- Improved Glycemic Control: By delivering insulin continuously and offering precise mealtime insulin dosing, insulin pump therapy can help individuals achieve tighter glycemic control and reduce fluctuations in blood glucose levels.
- Reduced Hypoglycemia: Insulin pump therapy enables fine-tuning of insulin delivery to match insulin requirements more closely, reducing the risk of hypoglycemia compared to fixed-dose insulin regimens.
Advanced insulin pump systems incorporate integrated CGM technology, allowing for sensor-augmented pump therapy (SAP) and automated insulin delivery algorithms (hybrid closed-loop systems) to optimize glycemic control and simplify diabetes management.
4. Carbohydrate Counting and Meal Planning
Carbohydrate counting, also known as carbohydrate counting, is a fundamental skill for individuals with type 1 diabetes, allowing them to match insulin doses with carbohydrate intake and optimize postprandial glucose control. Carbohydrate counting involves estimating the carbohydrate content of foods and beverages and adjusting insulin doses accordingly using an insulin-to-carbohydrate ratio (ICR) prescribed by a healthcare provider.
In addition to carbohydrate counting, meal planning plays a crucial role in type 1 diabetes management, focusing on balanced nutrition, portion control, and timing of meals and snacks to maintain stable blood glucose levels throughout the day. Healthcare providers, dietitians, and certified diabetes educators (CDEs) work collaboratively with individuals with type 1 diabetes to develop personalized meal plans that align with their dietary preferences, cultural background, and treatment goals.
5. Exercise and Physical Activity
Regular exercise and physical activity are integral components of type 1 diabetes management, offering numerous health benefits, including improved insulin sensitivity, weight management, cardiovascular health, and stress reduction. However, physical activity can also affect blood glucose levels, requiring careful planning and monitoring to prevent hypoglycemia or hyperglycemia during and after exercise.
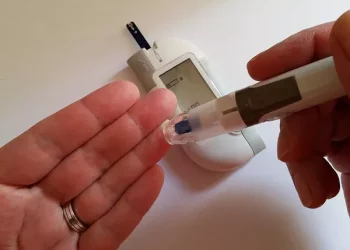
Individuals with type 1 diabetes are encouraged to incorporate a variety of physical activities into their daily routine, including aerobic exercise, strength training, flexibility exercises, and recreational activities. Prior to engaging in physical activity, it is essential to check blood glucose levels, consume appropriate snacks or carbohydrates as needed, and adjust insulin doses or basal rates as recommended by a healthcare provider.
6. Education, Support, and Self-Management
Education, support, and self-management skills are critical for individuals with type 1 diabetes to navigate the complexities of their condition, make informed decisions, and maintain optimal health and well-being. Comprehensive diabetes education programs, led by healthcare providers, certified diabetes educators (CDEs), and multidisciplinary teams, offer valuable resources and support to empower individuals with type 1 diabetes and their caregivers.
Key components of diabetes education and support include:
- Diabetes Self-Management Education (DSME): DSME programs provide individuals with type 1 diabetes with the knowledge, skills, and tools to manage their condition effectively, including insulin therapy, blood glucose monitoring, carbohydrate counting, meal planning, exercise, and stress management.
- Psychosocial Support: Living with type 1 diabetes can have a significant emotional and psychosocial impact on individuals and their families. Psychosocial support services, such as individual counseling, support groups, and peer mentorship programs, offer opportunities for individuals to connect with others, share experiences, and receive emotional support and encouragement.
- Continuous Monitoring and Follow-Up: Regular monitoring and follow-up with healthcare providers are essential to track progress, adjust treatment plans, address challenges or concerns, and prevent complications. Healthcare providers collaborate with individuals with type 1 diabetes to set personalized goals, monitor key health indicators, and optimize diabetes management strategies over time.
Conclusion: Optimizing Care and Empowering Individuals
In conclusion, type 1 diabetes management encompasses a multifaceted approach that integrates various treatment modalities, including insulin therapy, continuous glucose monitoring, insulin pump therapy, carbohydrate counting, meal planning, exercise, education, support, and self-management skills. By employing a comprehensive and individualized approach to care, healthcare providers can empower individuals with type 1 diabetes to achieve optimal glycemic control, minimize the risk of complications, and enhance their quality of life. Through ongoing education, support, and collaboration, individuals with type 1 diabetes can navigate the challenges of their condition with confidence and resilience, living full and active lives while effectively managing their diabetes.