In the intricate landscape of diabetes mellitus, type 2 diabetes stands as a pervasive and multifaceted condition characterized by insulin resistance, impaired glucose metabolism, and a host of metabolic abnormalities.
Among the myriad complications and manifestations of type 2 diabetes, polyuria emerges as a common and often perplexing symptom, leaving individuals grappling with frequent and excessive urination.
In this comprehensive exploration, we unravel the underlying mechanisms and complexities of polyuria in type 2 diabetes, shedding light on its causes, consequences, and implications for diabetes management and well-being.
Understanding Polyuria
Polyuria, a hallmark symptom of diabetes, refers to the passage of abnormally large volumes of urine, exceeding 2.5 liters per day in adults.
While polyuria can occur in various medical conditions and physiological states, its association with diabetes, particularly type 2 diabetes, underscores the intricate interplay between glucose metabolism, fluid balance, and renal function.
The Role of Glucose in Polyuria
At the heart of polyuria in type 2 diabetes lies the dysregulation of glucose metabolism and its repercussions on renal physiology. In individuals with uncontrolled or poorly managed type 2 diabetes, elevated blood sugar levels spill over into the urine through the process of glucosuria, whereby the kidneys excrete excess glucose to maintain blood sugar homeostasis.
This phenomenon, known as renal threshold for glucose, occurs when blood glucose levels surpass the kidneys’ capacity to reabsorb glucose back into the bloodstream, leading to its excretion in the urine.
Osmotic Diuresis
The presence of glucose in the urine sets off a cascade of events within the renal tubules, culminating in osmotic diuresis—the primary mechanism underlying polyuria in type 2 diabetes.
As glucose-rich urine passes through the renal tubules, it creates an osmotic gradient that draws water out of the bloodstream and into the urine, resulting in increased urine volume and frequency of urination. This osmotic diuresis contributes to dehydration, electrolyte imbalances, and a heightened risk of urinary tract infections in individuals with uncontrolled type 2 diabetes.
Impact on Fluid Balance and Renal Function
The relentless cycle of polyuria and osmotic diuresis exerts a significant toll on fluid balance and renal function, disrupting the kidneys’ ability to concentrate urine and conserve water.
Chronic exposure to hyperglycemia and dehydration can lead to renal hypertrophy, impaired tubular function, and progressive kidney damage—a phenomenon known as diabetic nephropathy.
Additionally, the loss of water and electrolytes through polyuria can precipitate electrolyte imbalances, such as hyponatremia (low sodium levels) and hypokalemia (low potassium levels), further exacerbating metabolic disturbances in individuals with type 2 diabetes.
Consequences and Clinical Implications
The consequences of polyuria in type 2 diabetes extend beyond its immediate impact on urinary frequency and fluid balance, encompassing a spectrum of clinical implications and health risks:
1. Dehydration and Electrolyte Imbalances:
Prolonged or severe polyuria can lead to dehydration, electrolyte imbalances, and disturbances in acid-base balance, increasing the risk of complications such as hypovolemic shock, muscle cramps, and cardiac arrhythmias.
2. Urinary Tract Infections:
The dilution of urine and alterations in urinary pH associated with polyuria create an environment conducive to the growth of bacteria, raising the risk of urinary tract infections (UTIs) in individuals with type 2 diabetes. UTIs can lead to discomfort, pain, and systemic complications if left untreated, necessitating prompt diagnosis and management.
3. Impact on Quality of Life:
The disruptive nature of polyuria, characterized by frequent trips to the bathroom, nocturia (nighttime urination), and urgency, can significantly impact quality of life for individuals with type 2 diabetes, affecting sleep patterns, social activities, and daily routines.
4. Diagnostic Significance:
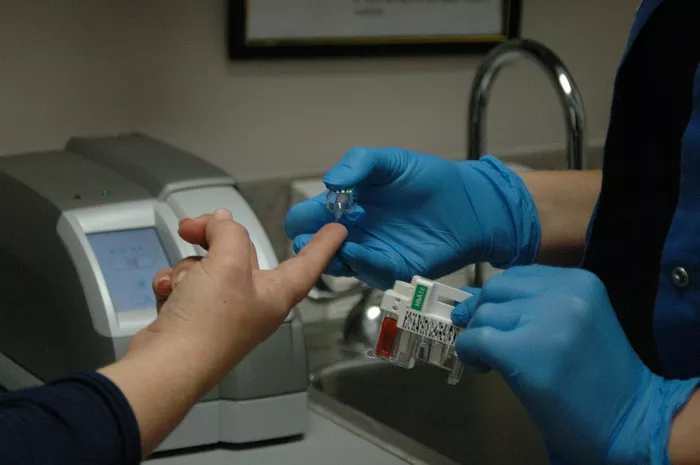
Polyuria serves as a cardinal symptom of diabetes and a key diagnostic criterion for identifying individuals at risk for or affected by the condition. Monitoring urinary output and fluid intake can provide valuable insights into glycemic control, kidney function, and overall health status in individuals with type 2 diabetes.
Strategies for Management and Mitigation
While polyuria remains a challenging aspect of diabetes management, several strategies can help individuals with type 2 diabetes mitigate its impact and optimize urinary health:
1. Glycemic Control:
Achieving and maintaining optimal blood sugar control through lifestyle modifications, medication adherence, and regular monitoring is paramount for reducing the severity and frequency of polyuria episodes in individuals with type 2 diabetes.
2. Hydration Management:
Encouraging adequate fluid intake, particularly water, can help counteract the effects of dehydration associated with polyuria and osmotic diuresis.
However, individuals with type 2 diabetes should be cautious about excessive fluid intake, especially if they have comorbidities such as heart failure or kidney disease.
3. Electrolyte Monitoring:
Regular monitoring of electrolyte levels, including sodium, potassium, and chloride, can help detect and address imbalances associated with polyuria and osmotic diuresis. Dietary modifications, electrolyte supplements, and medication adjustments may be necessary to restore electrolyte balance and prevent complications.
4. Renal Function Assessment:
Routine assessment of renal function, including kidney function tests, urine albumin-to-creatinine ratio (ACR), and estimated glomerular filtration rate (eGFR), is essential for identifying early signs of diabetic nephropathy and guiding appropriate management strategies to preserve kidney function.
5. Individualized Care Plans:
Collaborating with healthcare providers to develop individualized care plans tailored to the unique needs, preferences, and goals of each individual with type 2 diabetes is critical for optimizing diabetes management and minimizing the impact of polyuria on quality of life.
Conclusion
In conclusion, polyuria represents a common and often challenging symptom of type 2 diabetes, stemming from the dysregulation of glucose metabolism, fluid balance, and renal function.
By understanding the underlying mechanisms and consequences of polyuria, individuals with type 2 diabetes, along with their healthcare providers, can implement targeted strategies for managing and mitigating its impact on urinary health and overall well-being.
Through a multifaceted approach encompassing glycemic control, hydration management, electrolyte monitoring, renal function assessment, and individualized care planning, individuals with type 2 diabetes can navigate the complexities of polyuria with greater confidence and resilience.
As our understanding of type 2 diabetes and its associated complications continues to evolve, ongoing research, education, and innovation hold the promise of improving outcomes and enhancing the quality of life for millions affected by this prevalent and pervasive chronic condition.