In the intricate tapestry of diabetes management, hypoglycemia emerges as a formidable adversary, casting a shadow of uncertainty and fear over the lives of millions affected by the condition.
Defined as abnormally low blood sugar levels, hypoglycemia poses a significant threat to health and well-being, with potentially dire consequences if left unaddressed.
In this comprehensive exploration, we delve into the dangers of hypoglycemia, unraveling its causes, manifestations, and far-reaching implications for individuals living with diabetes.
Understanding Hypoglycemia
Hypoglycemia, often referred to as a “hypo,” occurs when blood sugar levels drop below normal range, typically defined as less than 70 milligrams per deciliter (mg/dL).
Under normal circumstances, the body tightly regulates blood sugar levels through a delicate balance of insulin and glucagon, hormones that work in tandem to maintain glucose homeostasis. However, in individuals with diabetes, this balance can be disrupted, leading to episodes of hypoglycemia.
Why Hypoglycemia Occurs
Hypoglycemia can occur for various reasons, with the underlying mechanisms differing between individuals with type 1 diabetes, type 2 diabetes, and other forms of diabetes. Some common causes of hypoglycemia include:
1. Excessive Insulin or Diabetes Medications:
In individuals with diabetes who take insulin or certain oral medications to lower blood sugar levels, hypoglycemia can occur if too much medication is administered, or if insulin doses are not adjusted appropriately in response to changes in diet, physical activity, or insulin sensitivity.
2. Delayed or Missed Meals:
Skipping meals, delaying meals, or not consuming enough carbohydrates to match insulin doses can lead to hypoglycemia, particularly in individuals with diabetes who are taking insulin or other glucose-lowering medications.
3. Intense Physical Activity:
Strenuous exercise or prolonged physical activity can increase the body’s demand for glucose, leading to hypoglycemia if adequate carbohydrate intake or adjustments to insulin doses are not made beforehand.
4. Alcohol Consumption:
Consuming alcohol, especially on an empty stomach or in large quantities, can impair the liver’s ability to release stored glucose and increase the risk of hypoglycemia, particularly in individuals with diabetes who are taking insulin or other glucose-lowering medications.
5. Changes in Hormone Levels:
Hormonal fluctuations, such as those that occur during puberty, menstruation, pregnancy, or menopause, can affect insulin sensitivity and glucose metabolism, potentially leading to hypoglycemia in individuals with diabetes.
6. Medical Conditions or Medications:
Certain medical conditions, such as kidney or liver disease, adrenal insufficiency, or infections, as well as certain medications, can interfere with glucose regulation and increase the risk of hypoglycemia in individuals with diabetes.
The Dangers of Hypoglycemia
Hypoglycemia can manifest with a wide range of symptoms, varying in severity depending on the degree and duration of low blood sugar levels. Common symptoms of hypoglycemia include:
- Shakiness
- Sweating
- Palpitations
- Hunger
- Irritability or mood changes
- Confusion or difficulty concentrating
- Dizziness or lightheadedness
- Headache
- Blurred vision
- Weakness or fatigue
- Seizures
- Loss of consciousness (in severe cases)
In addition to the immediate symptoms of hypoglycemia, repeated or severe episodes can have serious consequences for health and well-being, including:
1. Impaired Cognitive Function:
Hypoglycemia can impair cognitive function and decision-making abilities, potentially leading to accidents, falls, or other safety concerns, particularly in individuals who operate heavy machinery or engage in activities that require mental alertness.
2. Increased Risk of Cardiovascular Events:
Severe hypoglycemia has been associated with an increased risk of cardiovascular events, such as heart attack, stroke, or arrhythmias, particularly in individuals with pre-existing cardiovascular disease or risk factors.
3. Reduced Quality of Life:
The fear of hypoglycemia and the need to constantly monitor blood sugar levels can significantly impact quality of life for individuals with diabetes and their families. Fear of hypoglycemia may lead to avoidance of physical activity, social isolation, anxiety, depression, and decreased adherence to diabetes management regimens.
4. Hypoglycemia Unawareness:
In some cases, individuals with diabetes may develop hypoglycemia unawareness, a condition characterized by a reduced ability to recognize the symptoms of low blood sugar. This can increase the risk of severe hypoglycemia and its associated complications, as prompt treatment may be delayed or omitted.
5. Brain Damage or Death:
Severe or prolonged hypoglycemia can lead to irreversible brain damage or death if left untreated.
Severe hypoglycemia requiring assistance from another person to treat, also known as severe hypoglycemia with impaired consciousness (SHiC), is a medical emergency that requires immediate intervention with oral glucose or intravenous dextrose to raise blood sugar levels.
Preventing and Managing Hypoglycemia
While hypoglycemia poses significant challenges for individuals living with diabetes, several strategies can help prevent and manage hypoglycemic episodes:
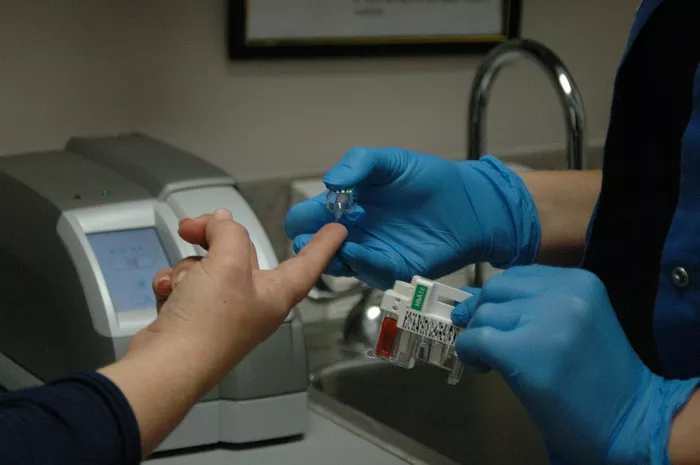
1. Regular Blood Sugar Monitoring:
Regular monitoring of blood sugar levels, particularly before and after meals, physical activity, and bedtime, can help identify patterns and trends in blood sugar control and detect early signs of hypoglycemia.
2. Balanced Nutrition:
Consuming regular meals and snacks that are balanced in carbohydrates, protein, and fat can help stabilize blood sugar levels and reduce the risk of hypoglycemia. Carrying fast-acting sources of glucose, such as glucose tablets or gel, can provide a quick and convenient way to treat hypoglycemia if it occurs.
3. Individualized Treatment Plans:
Working closely with healthcare providers to develop individualized treatment plans based on factors such as age, medical history, lifestyle, and treatment goals can help optimize blood sugar control and minimize the risk of hypoglycemia.
4. Medication Management:
Adjusting insulin doses, timing, and formulations, as well as carefully titrating other glucose-lowering medications, can help prevent hypoglycemia while maintaining optimal blood sugar control.
Continuous glucose monitoring (CGM) systems and insulin pump therapy offer advanced tools for monitoring blood sugar levels and delivering insulin with greater precision.
5. Education and Support:
Providing individuals with diabetes and their families with comprehensive education and support on hypoglycemia recognition, prevention, and treatment is essential for effective diabetes management.
Peer support networks, diabetes education programs, and online resources can offer valuable insights, practical tips, and emotional support for navigating the challenges of living with diabetes.
Conclusion
In conclusion, hypoglycemia represents a significant and potentially life-threatening complication for individuals living with diabetes. With its diverse manifestations, ranging from mild symptoms of shakiness and sweating to severe consequences such as impaired cognitive function, cardiovascular events, and even death, hypoglycemia demands vigilance, awareness, and proactive management.
By understanding the causes, manifestations, and consequences of hypoglycemia, individuals with diabetes can take proactive steps to prevent and manage hypoglycemic episodes, optimize blood sugar control, and safeguard their health and well-being.
As our understanding of hypoglycemia continues to evolve, ongoing research, innovation, and collaboration hold the promise of improving outcomes and enhancing the quality of life for individuals affected by this challenging and pervasive complication of diabetes.