Blood sugar, also referred to as blood glucose, plays a critical role in the body’s functioning. Our body relies on glucose as a key energy source for cells, tissues, and organs. The body maintains blood glucose levels within a narrow range through a complex interaction of hormones, enzymes, and other biochemical pathways. However, when blood sugar levels go too high or too low, it can pose a significant risk to health, leading to a range of potential complications. This article explores what is considered a dangerous blood sugar level, the factors influencing it, the symptoms of abnormal blood sugar levels, and how to manage these levels to prevent serious health consequences.
Understanding Blood Sugar Levels
Before delving into what constitutes a dangerous blood sugar level, it is crucial to understand how normal blood sugar levels are measured and what the typical ranges are. Blood sugar levels fluctuate throughout the day, depending on factors such as the time since the last meal, physical activity, and stress levels. However, general guidelines can help establish what is considered normal, elevated, or low.
Normal Blood Sugar Levels: According to the American Diabetes Association (ADA), the normal range for fasting blood glucose (measured after at least 8 hours of fasting) is between 70 and 99 mg/dL. Post-meal blood glucose levels should ideally be below 140 mg/dL two hours after eating.
Pre-diabetes: When blood glucose levels consistently range between 100 mg/dL and 125 mg/dL while fasting, this indicates a condition known as pre-diabetes. Pre-diabetes is a risk factor for developing type 2 diabetes, but it is not classified as a dangerous blood sugar level yet. Nevertheless, it requires monitoring and lifestyle changes to prevent progression.
Diabetes: A diagnosis of diabetes is made when fasting blood glucose levels are consistently 126 mg/dL or higher. In addition, post-meal blood sugar levels higher than 200 mg/dL two hours after eating are indicative of diabetes. People with diabetes must manage their blood sugar levels closely to avoid dangerous extremes.
Dangerously High Blood Sugar (Hyperglycemia)
Hyperglycemia, or high blood sugar, is a condition that occurs when blood glucose levels are consistently too high. This condition is common in individuals with diabetes, but it can also occur in people who do not have diabetes, especially during times of illness, stress, or poor dietary habits. Hyperglycemia can be mild, moderate, or severe, and each level carries its own risks.
Mild Hyperglycemia: Blood glucose levels between 140 mg/dL and 180 mg/dL are considered mildly elevated and can occur after eating a meal. While these levels may not immediately pose a significant risk, they still require attention to prevent further increase and complications.
Moderate Hyperglycemia: Blood glucose levels ranging from 180 mg/dL to 250 mg/dL are more concerning, and individuals should take corrective measures such as adjusting insulin or medication, increasing physical activity, or altering their diet to bring levels back down into the normal range.
Severe Hyperglycemia (Dangerous Highs): Blood glucose levels that exceed 250 mg/dL are considered dangerously high and can lead to severe health complications. Persistent high blood sugar can damage organs, tissues, and blood vessels over time, increasing the risk of heart disease, kidney failure, nerve damage, and blindness. When blood glucose levels are exceedingly high, it can lead to a life-threatening condition called diabetic ketoacidosis (DKA), which requires immediate medical intervention.
Diabetic Ketoacidosis (DKA)
Diabetic ketoacidosis is a medical emergency that primarily affects people with type 1 diabetes but can also occur in individuals with type 2 diabetes. DKA occurs when the body starts to break down fat for energy due to an insufficient supply of insulin, leading to the production of ketones, which can accumulate in the blood and cause it to become acidic. Symptoms of DKA include:
-
Nausea and vomiting
-
Abdominal pain
-
Difficulty breathing (rapid, deep breathing)
-
Fruity-smelling breath
-
Confusion or disorientation
DKA requires immediate treatment, often in a hospital setting, involving insulin administration, intravenous fluids, and electrolyte management.
Dangerously Low Blood Sugar (Hypoglycemia)
On the opposite end of the spectrum, hypoglycemia refers to dangerously low blood sugar levels. A blood glucose level below 70 mg/dL is generally considered hypoglycemic. While many people experience occasional dips in blood glucose, prolonged or severe hypoglycemia can be life-threatening. Individuals with diabetes who are on insulin or other medications that lower blood glucose are at a higher risk of experiencing hypoglycemia.
Mild Hypoglycemia: Symptoms of mild hypoglycemia include shakiness, sweating, rapid heartbeat, hunger, and irritability. At this level, individuals can often self-treat by consuming fast-acting carbohydrates, such as glucose tablets, fruit juice, or regular soda.
Moderate Hypoglycemia: When blood glucose levels fall further, typically below 50 mg/dL, symptoms can worsen, including confusion, dizziness, weakness, blurred vision, and difficulty concentrating. At this point, a prompt intervention is necessary, and an individual may need assistance from a caregiver or healthcare professional.
Severe Hypoglycemia: Severe hypoglycemia occurs when blood glucose levels drop below 20-30 mg/dL. This can lead to loss of consciousness, seizures, or even death if not treated immediately. People experiencing severe hypoglycemia require an emergency injection of glucagon or intravenous glucose administered by a medical professional.
The Role of Insulin and Other Medications in Blood Sugar Control
For people with diabetes, the most common method of managing blood sugar levels is through the use of insulin and other medications. Insulin helps the body use glucose by facilitating its entry into cells, where it is used for energy. There are different types of insulin (rapid-acting, long-acting, intermediate, and short-acting), each with varying durations of action.
Insulin Therapy: For individuals with type 1 diabetes and some individuals with type 2 diabetes, insulin therapy is essential. Adjusting insulin doses based on food intake, physical activity, and stress levels is critical for avoiding both hyperglycemia and hypoglycemia.
Oral Medications: For type 2 diabetes, various oral medications help manage blood sugar levels. These medications include metformin, sulfonylureas, and SGLT2 inhibitors. While they may help control blood sugar, they are typically not sufficient on their own, and insulin therapy may be required in some cases.
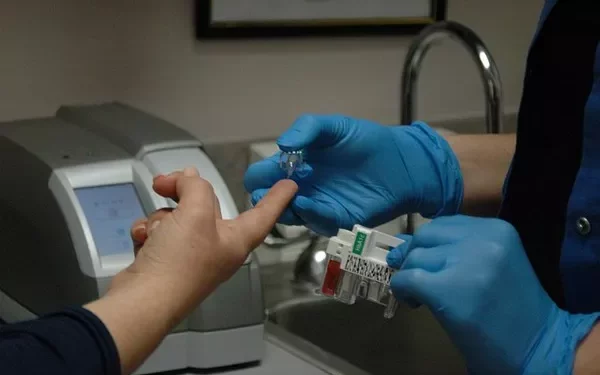
Continuous Glucose Monitoring (CGM): For individuals who require close monitoring, continuous glucose monitoring systems can provide real-time data on blood glucose levels. CGMs help people with diabetes make timely adjustments to their diet, exercise, and medications to maintain blood sugar levels within a safe range.
Managing Blood Sugar Levels to Avoid Dangerous Extremes
Proper management of blood glucose is the key to preventing dangerous blood sugar levels. Individuals with diabetes or pre-diabetes should work closely with their healthcare team to establish a tailored plan for blood sugar control.
Diet: Consuming a balanced diet that includes complex carbohydrates, lean proteins, and healthy fats can help regulate blood sugar levels. Avoiding large quantities of sugary foods and refined carbohydrates is essential in preventing blood sugar spikes.
Exercise: Regular physical activity helps the body use insulin more effectively and can lower blood sugar levels. However, individuals should be cautious and monitor their blood sugar levels closely during exercise, as physical activity can also lead to hypoglycemia.
Medication Adherence: Following prescribed medication regimens, whether insulin or oral drugs, is crucial for managing blood sugar levels. Skipping doses or improper use of medications can result in dangerous fluctuations in blood glucose.
Stress Management: Chronic stress can elevate blood sugar levels by releasing stress hormones like cortisol. Managing stress through relaxation techniques, mindfulness, or other coping strategies is essential for maintaining stable blood sugar levels.
Conclusion
A dangerous blood sugar level is a serious health concern, whether it involves dangerously high blood sugar (hyperglycemia) or dangerously low blood sugar (hypoglycemia). Both extremes can lead to immediate and long-term health complications. Early detection, regular monitoring, and proactive management are essential in preventing these dangerous levels and minimizing the risk of complications. People with diabetes should work closely with their healthcare providers to maintain optimal blood glucose levels through lifestyle changes, medications, and regular blood sugar monitoring. By staying vigilant and informed, individuals can better manage their blood sugar and lead a healthier, more balanced life.
Related topics:
What Makes Blood Glucose Levels Go Down?