In a breakthrough that could transform the treatment of diabetes, researchers at the University of Geneva have identified a protein, S100A9, which has shown potential to replace insulin therapy for some patients, reducing the risk of life-threatening complications like diabetic ketoacidosis (DKA).
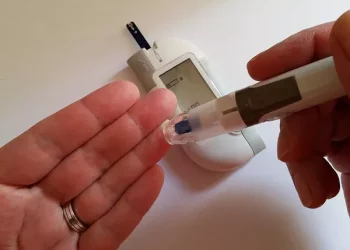
For those with type 1 diabetes, insulin injections are vital for managing blood sugar levels. However, the therapy is not without its drawbacks—insulin is difficult to dose, and overuse can result in hypoglycemia, long-term metabolic issues, and a shortened lifespan. For decades, insulin has been the primary treatment, with no alternative capable of managing the dangerous build-up of ketones in the body.
Enter S100A9. Discovered by Professor Roberto Coppari and his team, S100A9 has demonstrated the ability to manage blood sugar, ketone levels, and lipid profiles in diabetic mice—all without the need for insulin. This breakthrough raises the possibility of a safer, more effective treatment for diabetes that could potentially reduce or replace insulin use.
The body naturally produces ketones as a backup energy source during food scarcity. However, in individuals with insulin deficiency, such as those with type 1 diabetes, ketone production can spiral out of control, leading to a dangerous acid build-up in the blood known as DKA. Each year, between 2-4% of type 1 diabetes patients experience DKA, a condition that can be fatal if untreated.
S100A9 works by activating a receptor called Toll-like receptor 4 (TLR4) in the liver, which in turn regulates ketone production. Remarkably, this process doesn’t trigger inflammation, despite TLR4’s usual role in immune responses. This discovery could offer a dual benefit: regulating ketone levels and potentially offering anti-inflammatory effects.
“We’ve discovered that S100A9 can suppress ketone production in the liver without causing the inflammation typically associated with TLR4 activation,” explained Gloria Ursino, a key researcher on the project. “This could pave the way for a new class of anti-inflammatory treatments.”
The team’s findings, published in Nature Communications, highlight how S100A9 could be administered through injections, possibly reducing ketone levels and improving glucose regulation without triggering hypoglycemia—a common risk of insulin therapy. Tests in diabetic mice showed that the protein not only lowered ketone levels but also helped insulin-deprived mice live longer.
With CHF 2.5 million in funding from the Helmsley Charitable Trust, the research team is now preparing for clinical trials. The grant will fund preclinical studies and move the team closer to human testing, with trials expected to begin in 2025.
“We believe that S100A9 could change how we approach diabetes treatment,” said Giorgio Ramadori, a senior lecturer at the University of Geneva. “This funding is crucial to moving the project forward and potentially improving the lives of millions of people living with type 1 diabetes.”
This discovery comes as current diabetes treatments primarily focus on improving insulin sensitivity, but still rely on insulin, which carries its own set of risks. S100A9 represents a shift in this paradigm, as it works independently of insulin and could eventually reduce the body’s dependence on it.
The protein’s potential doesn’t stop at diabetes. S100A9’s ability to regulate metabolism without triggering inflammation may offer benefits for other conditions associated with poor metabolism and inflammation. Researchers are optimistic that this approach could extend beyond diabetes and offer new treatment avenues for various inflammatory diseases.
To further develop S100A9 as a therapeutic option, the research team has launched Diatheris, a startup company dedicated to turning this discovery into a viable treatment. Supported by the University of Geneva’s technology transfer office and regional innovation funds, Diatheris aims to bring S100A9 to market.
With clinical trials on the horizon, the S100A9 protein could soon offer a groundbreaking alternative to insulin therapy, providing a safer, more effective way for diabetes patients to manage their condition and potentially changing the landscape of diabetes care forever.
Related topics:
Over 250 Million People Globally Unaware of Their Diabetes Diagnosis
Vitamin C from Fresh Foods May Lower Heart Disease Risk in Type 2 Diabetes Patients
Early Lifestyle Choices Lead to Rising Health Risks in Young Adults, Experts Warn