The concept of borderline diabetes, often referred to as prediabetes, is a crucial term in the world of diabetes management. It represents a state where an individual’s blood glucose levels are higher than normal but not high enough to qualify for a diabetes diagnosis. Understanding what constitutes a borderline diabetic reading is essential for early intervention and lifestyle modifications to prevent the progression to type 2 diabetes. This article explores what borderline diabetic readings mean, how they are diagnosed, and the implications of such a diagnosis for long-term health.
Introduction: The Rising Prevalence of Prediabetes
Diabetes has become one of the most prevalent chronic conditions globally, with an increasing number of people being diagnosed each year. However, not everyone who is at risk immediately develops full-blown diabetes. The concept of prediabetes—where a person’s blood sugar levels are elevated but not yet in the diabetic range—has gained significant attention as a critical marker for early intervention.
Prediabetes is often an asymptomatic condition, meaning that many individuals may not even be aware that their blood glucose levels are outside the normal range. Borderline diabetic readings are a wake-up call, signaling that it’s time to adopt preventive strategies to reduce the likelihood of developing type 2 diabetes.
Understanding the Criteria for Borderline Diabetic Readings
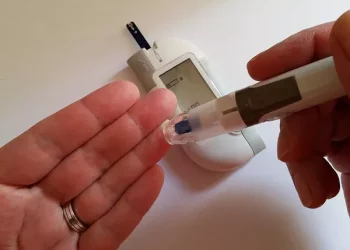
Borderline diabetic readings are not based on a single test but on a combination of tests and measurements that indicate an individual is at increased risk of developing type 2 diabetes. The main diagnostic tools used to identify borderline diabetes include the fasting blood glucose test, the oral glucose tolerance test (OGTT), and the hemoglobin A1c test.
Fasting Blood Glucose Test
A fasting blood glucose test measures the level of glucose in the blood after an overnight fast. The normal range for fasting blood glucose is typically between 70 and 100 milligrams per deciliter (mg/dL). If the fasting blood glucose is between 100 and 125 mg/dL, this is classified as prediabetes or a borderline diabetic reading. A reading of 126 mg/dL or higher on two separate tests indicates diabetes.
Oral Glucose Tolerance Test (OGTT)
The OGTT involves drinking a glucose solution after fasting overnight. Blood glucose levels are tested two hours later. A normal reading is less than 140 mg/dL. If the two-hour glucose level is between 140 and 199 mg/dL, the individual is considered to have prediabetes. A reading of 200 mg/dL or higher confirms diabetes.
Hemoglobin A1c Test
The A1c test measures the average blood glucose levels over the past two to three months. An A1c level between 5.7% and 6.4% is considered borderline or prediabetic. An A1c level of 6.5% or higher is used for a diagnosis of diabetes.
The Significance of Borderline Diabetic Readings
A borderline diabetic reading is a critical indicator that something may be off with your body’s ability to regulate blood glucose, but it’s not a definitive diagnosis of diabetes. It serves as a warning sign, offering an opportunity for intervention before the condition progresses into full-blown type 2 diabetes.
People with borderline diabetic readings are at a significantly higher risk of developing diabetes compared to those with normal blood sugar levels. In fact, the Centers for Disease Control and Prevention (CDC) estimates that about 1 in 3 American adults has prediabetes, and 90% of them are unaware of their condition.
Importantly, people with borderline diabetic readings can take proactive steps to reduce their risk, and in some cases, may even reverse the condition through lifestyle changes.
Risk Factors for Borderline Diabetes
Certain lifestyle factors and genetic predispositions can increase the likelihood of developing borderline diabetes. Understanding these risk factors is essential in recognizing those at greater risk for elevated blood glucose levels.
1. Obesity
Excess body fat, particularly abdominal fat, is one of the most significant risk factors for developing borderline diabetes. Fat cells are believed to interfere with the body’s ability to use insulin efficiently, leading to insulin resistance and higher blood glucose levels. A body mass index (BMI) over 25 is often associated with prediabetes.
2. Physical Inactivity
Physical activity helps to regulate blood glucose levels by enhancing insulin sensitivity. A sedentary lifestyle can contribute to weight gain, insulin resistance, and ultimately, prediabetes. The CDC recommends at least 150 minutes of moderate physical activity per week to help prevent diabetes.
3. Family History and Genetics
Having a first-degree relative (such as a parent or sibling) with diabetes increases an individual’s risk of developing prediabetes. Certain genetic factors also contribute to a higher risk, and individuals of specific ethnic backgrounds (including African American, Hispanic, Native American, and Asian American populations) are more likely to develop prediabetes.
4. Age
As people age, their risk of developing prediabetes increases. This may be due to the natural aging process, which can cause reduced insulin sensitivity and changes in body composition, such as an increase in abdominal fat. People over 45 years old should be more vigilant in monitoring their blood glucose levels.
5. Poor Diet
A diet high in processed foods, sugary beverages, and refined carbohydrates is a major contributor to the development of prediabetes. These foods can cause rapid spikes in blood glucose and over time, impair the body’s ability to regulate glucose levels effectively.
How Borderline Diabetic Readings Are Managed
The good news is that borderline diabetes can often be managed, and in some cases, even reversed. Early intervention is key to preventing progression to full-blown type 2 diabetes. The primary methods of managing borderline diabetic readings involve lifestyle changes, including diet and exercise.
1. Diet Modifications
Eating a balanced diet rich in whole foods, fiber, lean proteins, and healthy fats is one of the most effective strategies for managing borderline diabetes. Reducing intake of sugary foods, refined grains, and unhealthy fats is critical to stabilizing blood glucose levels.
Key dietary changes include:
Increase fiber intake: Fiber helps slow the absorption of sugar into the bloodstream, preventing spikes in blood glucose. Foods like fruits, vegetables, legumes, and whole grains are excellent sources of fiber.
Choose complex carbohydrates: Foods such as whole grains, sweet potatoes, and legumes provide slow-release energy and are absorbed more gradually, helping to maintain stable blood sugar levels.
Incorporate healthy fats: Healthy fats, such as those found in avocados, olive oil, and nuts, can improve insulin sensitivity.
Reduce sugary drinks: Sugary beverages, including sodas and fruit juices, can cause rapid spikes in blood glucose. Opt for water, unsweetened tea, or sparkling water with a splash of lemon.
2. Exercise and Physical Activity
Regular exercise is crucial for improving insulin sensitivity and controlling blood glucose levels. Physical activity helps the body use glucose more efficiently, reducing the amount of sugar in the bloodstream.
At least 150 minutes of moderate-intensity exercise per week (such as brisk walking, swimming, or cycling) can help reduce the risk of diabetes. Resistance training, such as weightlifting or bodyweight exercises, also plays a role in improving insulin sensitivity.
3. Weight Loss
Losing even a modest amount of weight can significantly reduce the risk of developing diabetes. For individuals who are overweight, losing 5-10% of body weight can have a meaningful impact on blood sugar levels. Weight loss helps improve insulin sensitivity and reduces fat accumulation around the organs, which is associated with insulin resistance.
Monitoring and Regular Checkups
If you’ve been diagnosed with borderline diabetes, regular monitoring of your blood glucose levels is essential. Your doctor may recommend more frequent blood tests to track changes in your glucose levels and assess the effectiveness of your lifestyle modifications.
In addition to blood glucose tests, regular checkups will help monitor other important health markers, such as blood pressure and cholesterol levels. These are often elevated in people with prediabetes and are important factors in the overall risk of cardiovascular disease, which is higher in individuals with diabetes.
The Role of Medications
In some cases, medications may be prescribed to help control blood sugar levels. Although lifestyle changes are the cornerstone of managing borderline diabetes, medications such as metformin may be used to improve insulin sensitivity and help regulate glucose levels. However, these should be seen as supplementary to lifestyle changes, not replacements.
Conclusion:
Borderline diabetic readings are a wake-up call, offering an opportunity for individuals to take control of their health before the onset of type 2 diabetes. By making thoughtful lifestyle changes, including adopting a healthy diet, exercising regularly, losing excess weight, and monitoring blood glucose levels, the progression to full-blown diabetes can often be prevented or delayed.
Understanding the signs and risks associated with borderline diabetes can empower individuals to make proactive decisions that protect their long-term health and well-being. Regular checkups, lifestyle interventions, and a commitment to better health can make all the difference in preventing the progression of this common and serious condition.
Related topics:
What is the Blood Test for Sugar Levels?