Diabetes is a complex and chronic condition that affects millions of people worldwide. The term “borderline diabetes” refers to a stage of glucose intolerance that is not yet classified as full-blown diabetes but is a warning sign that an individual is at an increased risk of developing type 2 diabetes. It is often also referred to as pre-diabetes or impaired glucose tolerance (IGT).
When blood glucose levels fall into a range that is higher than normal but not yet high enough to meet the criteria for diabetes, it is known as borderline diabetic numbers. This stage provides a critical window of opportunity to make lifestyle changes that can help prevent the progression to type 2 diabetes, a disease that can lead to complications such as heart disease, kidney failure, blindness, and neuropathy.
In this article, we will explore the concept of borderline diabetes, the diagnostic criteria used to identify it, the significance of blood glucose numbers, and most importantly, the steps that individuals can take to manage and possibly reverse this condition.
What Are Borderline Diabetic Numbers?
Borderline diabetic numbers refer to blood glucose levels that are higher than normal but do not yet meet the threshold for a diabetes diagnosis. These numbers are typically seen during routine blood glucose monitoring and can signal the early stages of impaired glucose metabolism. The most common ways of diagnosing borderline diabetes are through three key tests: the fasting blood glucose test, the oral glucose tolerance test (OGTT), and the hemoglobin A1c (HbA1c) test.
Diagnostic Criteria for Borderline Diabetes
There are specific ranges for each of these tests that help healthcare professionals determine if an individual is at risk of progressing to full diabetes. The following are the common thresholds for borderline diabetic numbers:
1. Fasting Blood Glucose Test (Fasting Plasma Glucose, FPG)
A fasting blood glucose test measures the level of glucose in the blood after an individual has fasted for at least 8 hours.
Normal Range: A fasting blood glucose level of less than 100 mg/dL (5.6 mmol/L) is considered normal.
Borderline (Pre-Diabetes) Range: A fasting blood glucose level between 100-125 mg/dL (5.6–6.9 mmol/L) indicates impaired fasting glucose (IFG), which is a sign of borderline diabetes.
Diabetic Range: A fasting blood glucose level of 126 mg/dL (7.0 mmol/L) or higher on two separate tests indicates diabetes.
A borderline result on the fasting blood glucose test suggests that the body is beginning to have trouble processing glucose, but it hasn’t yet reached the point of full diabetes.
2. Oral Glucose Tolerance Test (OGTT)
The OGTT is another common test for diagnosing borderline diabetes. It involves fasting overnight and then drinking a sugary solution. Blood glucose levels are measured before and two hours after consuming the solution.
Normal Range: A two-hour blood glucose level of less than 140 mg/dL (7.8 mmol/L) is considered normal.
Borderline (Pre-Diabetes) Range: A two-hour blood glucose level between 140-199 mg/dL (7.8–11.0 mmol/L) indicates impaired glucose tolerance (IGT), which is another marker for borderline diabetes.
Diabetic Range: A two-hour blood glucose level of 200 mg/dL (11.1 mmol/L) or higher indicates diabetes.
The OGTT is particularly useful for detecting impaired glucose tolerance, which is an early sign of diabetes.
3. Hemoglobin A1c Test (HbA1c)
The HbA1c test measures the average blood glucose level over the past two to three months. Unlike the fasting blood glucose test or the OGTT, it does not require fasting.
Normal Range: An HbA1c level of less than 5.7% is considered normal.
Borderline (Pre-Diabetes) Range: An HbA1c level between 5.7% and 6.4% indicates prediabetes.
Diabetic Range: An HbA1c level of 6.5% or higher on two separate tests indicates diabetes.
The HbA1c test is valuable because it provides a longer-term view of how well blood glucose is controlled, and it can help in identifying individuals with borderline diabetic numbers.
The Significance of Borderline Diabetic Numbers
Borderline diabetes is a warning sign. It does not mean that an individual has diabetes, but it indicates that their glucose metabolism is not functioning optimally. The significance of borderline diabetic numbers lies in the fact that this condition often precedes the development of type 2 diabetes. In fact, without intervention, many individuals with borderline diabetes will progress to type 2 diabetes within 5 to 10 years.
Studies show that people with borderline diabetes are at a higher risk of developing cardiovascular diseases, strokes, and kidney problems, among other complications. However, the good news is that borderline diabetes is manageable and, in many cases, reversible through lifestyle changes.
Risk Factors for Borderline Diabetes
Several risk factors can increase the likelihood of developing borderline diabetes. These include:
Age: Individuals over the age of 45 are more likely to develop borderline diabetes.
Family History: A family history of diabetes, particularly type 2 diabetes, increases the risk of developing borderline diabetes.
Obesity: Being overweight or obese is one of the most significant risk factors for developing insulin resistance, which can lead to borderline diabetes.
Physical Inactivity: Lack of physical activity can contribute to weight gain and insulin resistance, increasing the risk of developing glucose intolerance.
Unhealthy Diet: Diets high in processed foods, sugars, and unhealthy fats can impair glucose metabolism and increase the risk of borderline diabetes.
Gestational Diabetes: Women who had gestational diabetes during pregnancy are at a higher risk of developing borderline diabetes later in life.
High Blood Pressure: Having high blood pressure is another risk factor associated with insulin resistance and diabetes.
Managing Borderline Diabetes
The good news for individuals with borderline diabetic numbers is that the condition is often reversible or manageable with lifestyle changes. Here are the key steps that individuals can take to improve their health and reduce the risk of progressing to type 2 diabetes:
1. Dietary Changes
One of the most effective ways to manage borderline diabetes is by adopting a healthy, balanced diet. The goal is to stabilize blood sugar levels and improve insulin sensitivity. Key dietary strategies include:
Increase Fiber Intake: Fiber helps regulate blood sugar by slowing the absorption of glucose. High-fiber foods include vegetables, fruits, legumes, and whole grains.
Choose Low Glycemic Index Foods: Foods with a low glycemic index (GI) release glucose more slowly into the bloodstream. Examples include whole grains, beans, and non-starchy vegetables.
Reduce Processed Foods and Sugars: Avoid refined carbohydrates, sugary drinks, and processed foods, as these can cause rapid spikes in blood sugar.
Control Portion Sizes: Eating smaller, more frequent meals can help prevent large blood sugar fluctuations.
Incorporate Healthy Fats: Sources of healthy fats like avocados, nuts, and olive oil can improve insulin sensitivity.
2. Regular Physical Activity
Exercise plays a crucial role in managing borderline diabetes. Physical activity helps increase insulin sensitivity and promotes the use of glucose by muscles, which helps reduce blood sugar levels. The American Diabetes Association recommends at least 150 minutes per week of moderate-intensity aerobic exercise, such as brisk walking, swimming, or cycling, combined with strength training exercises at least two days a week.
3. Weight Management
Achieving and maintaining a healthy weight is one of the most effective ways to reduce the risk of progressing from borderline diabetes to full-blown type 2 diabetes. Even a modest weight loss of 5-10% of body weight can significantly improve blood glucose control and insulin sensitivity.
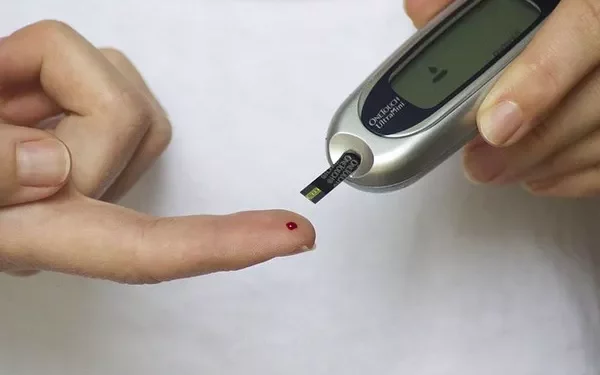
4. Regular Blood Glucose Monitoring
For individuals diagnosed with borderline diabetes, regular blood glucose monitoring is essential to track any changes in blood sugar levels. This can help identify patterns and enable timely interventions. Using a glucose meter or continuous glucose monitoring (CGM) device can provide valuable insights into how food, exercise, and other factors affect blood sugar levels.
5. Medication (If Necessary)
While lifestyle changes are the cornerstone of managing borderline diabetes, some individuals may need medication to help control blood glucose levels. Medications such as metformin may be prescribed to improve insulin sensitivity. However, medication should be viewed as a supplement to, not a replacement for, healthy lifestyle changes.
6. Regular Medical Check-ups
Individuals with borderline diabetes should have regular check-ups with their healthcare provider to monitor blood glucose levels, blood pressure, and cholesterol. In some cases, your doctor may recommend additional tests to assess for complications related to blood sugar control.
Conclusion
Borderline diabetes is a critical stage in the progression of type 2 diabetes. While individuals with borderline diabetic numbers are not yet diagnosed with diabetes, they are at increased risk of developing the condition in the future. However, with early intervention and lifestyle changes such as a balanced diet, regular exercise, weight management, and blood glucose monitoring, it is possible to prevent or delay the onset of type 2 diabetes.
For anyone with borderline diabetic numbers, the message is clear: take proactive steps now to protect your health and reduce your risk of developing more serious complications down the road. Regular check-ups, ongoing monitoring, and making small yet significant lifestyle changes can make all the difference in preventing the progression to diabetes and living a healthier life.
By understanding your body, maintaining healthy habits, and staying informed, you can take control of your health and ensure a better future.
Related topics: