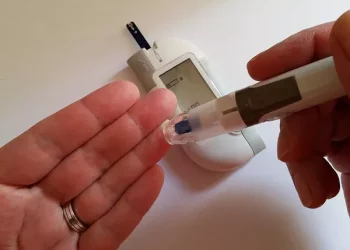
Hypoglycemia, or low blood sugar, is a condition characterized by abnormally low glucose levels in the bloodstream, typically below 70 mg/dL. This metabolic imbalance can trigger a range of unsettling symptoms, including dizziness, sweating, confusion, irritability, and in severe cases, loss of consciousness. While various factors can contribute to hypoglycemia, including certain medications and medical conditions, dietary choices play a pivotal role in both triggering and preventing these dangerous blood sugar crashes.
The Ultimate Hypoglycemia Diet
Hypoglycemia, commonly known as low blood sugar, occurs when glucose levels drop below the normal range, typically below 70 mg/dL. This condition can lead to unpleasant symptoms such as shakiness, sweating, confusion, and in severe cases, loss of consciousness. While medications can help manage hypoglycemia, dietary adjustments serve as the cornerstone of prevention and treatment. The ideal hypoglycemia diet focuses on maintaining steady glucose levels throughout the day by incorporating a strategic balance of macronutrients and carefully timed meals.
Understanding the Importance of Frequent, Balanced Meals
One of the most effective strategies for managing hypoglycemia involves eating small, frequent meals throughout the day. This approach prevents the blood sugar fluctuations that occur with traditional three-meal patterns. Ideally, individuals should consume five to six well-balanced meals or snacks spaced evenly every 3-4 hours. Each meal should contain a combination of complex carbohydrates, lean proteins, and healthy fats to ensure slow, sustained glucose release. This eating pattern helps avoid the rapid spikes and subsequent crashes that can trigger hypoglycemic episodes.
The Critical Role of Complex Carbohydrates
Complex carbohydrates form the foundation of a hypoglycemia-friendly diet due to their slow digestion rate. Unlike simple sugars that cause rapid glucose spikes, complex carbs provide a steady stream of energy. Excellent choices include whole grains like quinoa, brown rice, and whole wheat bread, which are rich in fiber and nutrients. Starchy vegetables such as sweet potatoes and squash also make excellent additions. These foods help maintain stable blood sugar levels while providing essential vitamins and minerals that support overall metabolic health.
Protein
Incorporating adequate protein at every meal is crucial for hypoglycemia management. Protein slows carbohydrate absorption, preventing the sudden blood sugar surges that can lead to reactive hypoglycemia. High-quality protein sources include lean meats like chicken and turkey, fatty fish rich in omega-3s, eggs, and plant-based options such as lentils and chickpeas. For optimal results, aim to include at least 15-20 grams of protein in each meal. This macronutrient not only stabilizes blood sugar but also promotes satiety, reducing the likelihood of overeating or reaching for unhealthy snacks.
Healthy Fats for Sustained Energy
Dietary fats play a vital role in hypoglycemia management by further slowing digestion and providing long-lasting energy. Focus on incorporating heart-healthy unsaturated fats from sources like avocados, nuts, seeds, and olive oil. These fats help create meals with a low glycemic impact while providing essential fatty acids that support cellular function. However, it’s important to moderate portion sizes, as fats are calorie-dense. A thumb-sized portion of nuts or a tablespoon of olive oil per meal provides sufficient fat without excessive calories.
The Hidden Dangers of Simple Sugars
Refined carbohydrates and simple sugars pose significant risks for individuals with hypoglycemia. These include white bread, pastries, sugary cereals, and sweetened beverages that cause rapid glucose spikes followed by crashes. Even seemingly healthy options like fruit juices can trigger hypoglycemic episodes due to their high sugar content and lack of fiber. When consuming fruits, opt for whole varieties with edible skins and pair them with protein or fat to moderate their glycemic impact. Reading nutrition labels carefully can help identify hidden sugars in processed foods.
Fiber
Dietary fiber serves as a powerful tool for blood sugar management. Soluble fiber, in particular, forms a gel-like substance in the digestive tract that slows carbohydrate absorption. Excellent sources include oats, legumes, flaxseeds, and many fruits and vegetables. Aim for at least 25-30 grams of fiber daily, gradually increasing intake to allow your digestive system to adjust. Fiber not only helps stabilize blood sugar but also promotes gut health and may improve insulin sensitivity over time.
Strategic Snacking for Blood Sugar Control
Well-planned snacks can prevent blood sugar dips between meals. The ideal hypoglycemia snack combines complex carbohydrates with protein and healthy fats. Some excellent options include apple slices with almond butter, whole grain crackers with cheese, or Greek yogurt with berries. Keep portable snacks readily available to address early warning signs of low blood sugar. A small snack before bedtime can also help prevent nocturnal hypoglycemia, particularly for those taking certain diabetes medications.
Hydration’s Role in Blood Sugar Stability
Proper hydration plays an often-overlooked role in blood sugar regulation. Dehydration can concentrate blood glucose levels and mimic hypoglycemia symptoms. Aim for at least eight glasses of water daily, increasing intake during hot weather or physical activity. Limit diuretics like caffeine and alcohol, which can contribute to fluid loss. For added benefit, infuse water with slices of citrus fruits or cucumber to enhance flavor without adding sugar.
The Glycemic Index
Understanding the glycemic index (GI) of foods can help make better dietary choices. Low-GI foods (55 or less) cause gradual blood sugar increases, while high-GI foods lead to rapid spikes. Many hypoglycemia-friendly foods naturally have low GI values, including most non-starchy vegetables, legumes, and whole grains. However, the glycemic response can vary based on food combinations, cooking methods, and individual metabolism. Pairing higher-GI foods with protein or fat can lower their overall glycemic impact.
Alcohol and Hypoglycemia
Alcohol consumption requires special consideration for those with hypoglycemia. Alcohol inhibits the liver’s ability to release glucose, increasing hypoglycemia risk. If choosing to drink, always consume alcohol with food and limit intake to moderate amounts. Avoid sugary mixed drinks that can cause blood sugar swings. Monitor blood glucose levels carefully when drinking, as alcohol can delay hypoglycemia symptoms, making them harder to recognize.
When to Consider Nutritional Supplements
Certain supplements may support blood sugar regulation, though they should never replace a balanced diet. Chromium picolinate may enhance insulin sensitivity, while magnesium plays a role in glucose metabolism. Cinnamon has shown potential in some studies for moderating blood sugar levels. Always consult a healthcare provider before starting supplements, especially if taking medications for diabetes or other conditions. Blood tests can identify specific nutrient deficiencies that may contribute to blood sugar instability.