High blood sugar, or hyperglycemia, is a prevalent and concerning health issue that affects millions worldwide. Left unmanaged, it can lead to a host of serious complications such as diabetes, heart disease, and nerve damage. While medical interventions are important, a growing body of scientific evidence points to diet as a powerful tool in effectively controlling blood sugar levels. This article delves into the science – backed dietary approach to managing high blood sugar, exploring every aspect from the impact of different food components to personalized nutrition strategies.
Understanding the Glycemic Impact of Foods
The cornerstone of blood sugar management lies in comprehending how different foods affect glucose levels. Foods with high glycemic index values cause rapid spikes in blood sugar, while low-GI alternatives provide a steady release of energy. It’s crucial to recognize that carbohydrate quality outweighs quantity – whole grains digest significantly slower than their refined counterparts. Soluble fiber plays a particularly important role by forming a gel-like substance in the digestive tract that slows carbohydrate absorption. Equally important is learning to identify hidden sugars in processed foods, which can sabotage blood sugar control efforts.
The Power of Non-Starchy Vegetables
Non-starchy vegetables should form the foundation of any blood sugar-friendly eating plan. Leafy greens like spinach and kale are rich in magnesium, a mineral that enhances insulin sensitivity. Cruciferous vegetables such as broccoli and cauliflower contain sulfur compounds that support the body’s natural detoxification processes. Colorful options including bell peppers and zucchini provide powerful antioxidants that help reduce oxidative stress. These vegetables offer high water and fiber content while contributing minimal carbohydrates, making them ideal for both blood sugar control and weight management.
Selecting the Right Carbohydrates
When managing high blood sugar, carbohydrate selection becomes paramount. Whole grains like quinoa and steel-cut oats retain their fiber-rich bran and germ, resulting in slower digestion. Legumes including lentils and chickpeas offer the dual benefit of plant-based protein and complex carbohydrates. Even starchy vegetables like sweet potatoes provide more nutrients and fiber than white potatoes. However, portion control remains essential – measuring servings using the plate method (filling half with non-starchy vegetables) helps maintain proper balance and prevent overconsumption.
Protein’s Crucial Role in Glucose Regulation
Adequate protein intake serves multiple functions in blood sugar management. It significantly slows gastric emptying, preventing the rapid absorption of glucose into the bloodstream. Protein also helps preserve lean muscle mass, which directly improves insulin sensitivity throughout the body. Furthermore, the satiety provided by protein-rich foods helps reduce cravings for sugary snacks. Plant-based proteins like tofu and tempeh offer excellent options, while fatty fish provide anti-inflammatory omega-3 fatty acids. Meat eaters should opt for lean cuts and remove visible fat to minimize inflammation risks.
Healthy Fats That Improve Insulin Function
Contrary to outdated beliefs, certain fats actively support metabolic health. Monounsaturated fats found in avocados and olives improve overall lipid profiles while enhancing insulin sensitivity. Omega-3 fatty acids from flaxseeds and walnuts reduce systemic inflammation that contributes to insulin resistance. Even medium-chain triglycerides in coconut oil may enhance fat metabolism. These healthy fats slow carbohydrate absorption while providing essential nutrients, though their high calorie density requires mindful portioning – typically a thumb-sized serving of nuts or one tablespoon of oil per meal.
Strategic Fruit Consumption
While fruits contain natural sugars, strategic selection and consumption can allow for their inclusion. Berries like blueberries and raspberries offer favorable fiber-to-sugar ratios that minimize glycemic impact. Citrus fruits provide valuable soluble fiber in their membranes when consumed whole. Apples and pears contain pectin that naturally moderates glucose release. Timing matters significantly – consuming fruit as part of meals rather than alone helps buffer its glycemic effect. However, dried fruits and juices should be limited due to their concentrated sugar content and reduced fiber.
Beverages That Support Glycemic Control
Hydration choices profoundly impact blood sugar regulation. Plain water remains the ideal choice with zero glycemic impact. Certain herbal teas, particularly those containing cinnamon or chamomile, may enhance insulin sensitivity. Black coffee, consumed in moderation, demonstrates protective effects against insulin resistance. Sugary drinks including fruit juices and sweetened teas should be avoided entirely. Even artificial sweeteners may disrupt glucose metabolism in sensitive individuals, making water the primary recommended beverage for optimal blood sugar control.
Spices and Herbs With Metabolic Benefits
Many common seasonings offer benefits beyond flavor enhancement. Cinnamon contains bioactive compounds that mimic insulin’s action in the body. Turmeric’s active component curcumin significantly reduces inflammation throughout the body. Ginger appears to enhance cellular glucose uptake through various mechanisms. These powerful spices can be easily incorporated into daily meals to boost both flavor and therapeutic value without adding calories or carbohydrates, making them valuable tools in blood sugar management.
Meal Timing and Frequency Considerations
The timing and frequency of meals significantly influence glycemic control. Maintaining consistent meal times helps regulate the body’s circadian rhythms and metabolic processes. For some individuals, smaller, more frequent meals may prevent the large glucose swings associated with larger, less frequent meals. Reducing carbohydrate intake in the evening aligns with the body’s natural circadian patterns of insulin sensitivity. Perhaps most importantly, avoiding late-night eating allows the pancreas necessary rest periods for optimal function and recovery.
Importance of Fiber Diversity
Different types of dietary fiber contribute uniquely to glucose control. Soluble fiber from psyllium and oats forms a viscous gel that slows carbohydrate absorption. Insoluble fiber from whole grains promotes healthy gut motility and regularity. Resistant starch, formed when certain cooked and cooled foods like potatoes are reheated, acts as a valuable prebiotic. Aiming for 25-35 grams of daily fiber from diverse sources supports both glycemic control and overall gut microbiome health, creating a synergistic effect for metabolic improvement.
Cooking Methods That Preserve Nutrient Value
Food preparation techniques significantly impact a meal’s glycemic effect. Steaming vegetables preserves their water-soluble nutrients better than boiling. Slow cooking methods help break down fibers in ways that may enhance their beneficial effects. Fermented foods like yogurt and kimchi provide probiotic benefits that support gut health. Conversely, deep-frying and high-temperature charring can create advanced glycation end products that may worsen insulin resistance, making these methods less desirable for blood sugar management.
Personalized Nutrition Approaches
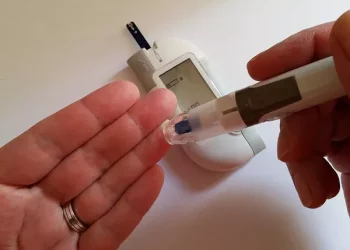
Individual factors play a crucial role in determining optimal dietary approaches. Genetic predispositions significantly affect carbohydrate tolerance between individuals. Activity levels and exercise patterns influence nutrient needs and utilization. Even gut microbiome composition impacts how nutrients are absorbed and metabolized. Continuous glucose monitoring technology now allows individuals to identify personal food triggers and determine appropriate portion sizes for different foods, enabling truly personalized nutrition strategies for blood sugar control.
Conclusion
Effective management of high blood sugar through diet requires a balanced, individualized approach focused on food quality rather than restrictive elimination. By emphasizing nutrient-dense whole foods, strategic macronutrient combinations, and mindful eating practices, individuals can achieve stable glucose levels while enjoying satisfying meals. The most successful dietary approach is one that can be maintained long-term while providing all necessary nutrients. Regular monitoring and gradual adjustments help fine-tune food choices for optimal metabolic health. Remember that dietary changes yield best results when combined with other lifestyle factors including physical activity and stress management for comprehensive blood sugar control.