Glucose serum level is a critical measurement in the field of healthcare, particularly for individuals living with diabetes and other metabolic conditions. It provides a snapshot of how much glucose, or sugar, is present in the blood at any given time. This measurement is a key factor in determining the overall health of an individual, as it directly reflects how well the body is managing and utilizing glucose. With rising rates of diabetes worldwide, understanding glucose serum levels is more important than ever.
This article aims to explain what glucose serum level is, why it is significant, and how it is measured. We will delve into the role glucose plays in the body, how it is regulated, and the implications of abnormal glucose levels. Special attention will be given to the relevance of glucose serum levels in the diagnosis and management of diabetes, as well as how healthcare providers use this data to adjust treatment plans and improve patient outcomes.
The Role of Glucose in the Body
Glucose is the primary source of energy for the body’s cells, particularly for the brain and muscles. When carbohydrates are consumed, they are broken down into glucose in the digestive system. This glucose is then absorbed into the bloodstream, where it circulates to provide fuel for the cells.
However, to use this glucose effectively, the body needs insulin—a hormone produced by the pancreas that allows glucose to enter cells. Insulin helps regulate glucose levels by facilitating its uptake into cells for energy production or storage as glycogen in the liver and muscles. This finely tuned system ensures that glucose is available when needed, but not in excess. When this system is disrupted, as is the case in diabetes, glucose levels can become imbalanced, leading to a variety of health complications.
What is Glucose Serum Level?
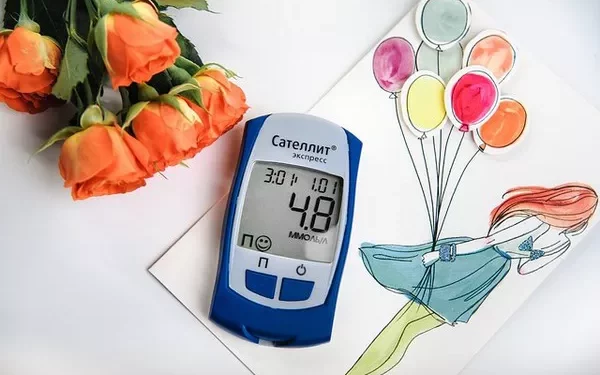
The term “glucose serum level” refers to the concentration of glucose in the liquid portion of blood, known as serum. Blood serum is the part of the blood that remains after the blood has clotted and the cells (like red blood cells and white blood cells) have been removed. Serum glucose levels are typically measured in milligrams per deciliter (mg/dL) in the United States, or millimoles per liter (mmol/L) in many other parts of the world.
Glucose serum levels are measured to assess how much glucose is circulating in the bloodstream at a given moment. This is a crucial metric for diagnosing and managing conditions such as diabetes, where the body’s ability to regulate glucose is impaired.
Normal Glucose Serum Levels
In healthy individuals, the glucose serum level is typically well-regulated and falls within a relatively narrow range. A normal glucose serum level indicates that the body is effectively processing and utilizing glucose. For individuals who do not have diabetes, the general guidelines for normal glucose serum levels are as follows:
Fasting Glucose: This is measured after at least 8 hours without eating. Normal fasting glucose levels generally range from 70 to 99 mg/dL (3.9 to 5.5 mmol/L).
Postprandial Glucose: This refers to glucose levels measured 2 hours after eating. Normal levels usually fall below 140 mg/dL (7.8 mmol/L).
Random Glucose: This is a measurement of glucose at any point throughout the day, regardless of when the individual last ate. Normal levels typically range between 70 and 140 mg/dL (3.9 to 7.8 mmol/L).
It’s important to note that glucose serum levels can fluctuate throughout the day due to various factors, including food intake, physical activity, stress, and illness. For individuals with diabetes or other health conditions, the target glucose serum level may differ and be tailored to their specific needs by their healthcare provider.
Abnormal Glucose Serum Levels: When to Be Concerned
Abnormal glucose serum levels—either too high (hyperglycemia) or too low (hypoglycemia)—can signal underlying health issues and may lead to long-term complications if left unchecked. Understanding these conditions is key to managing one’s health effectively.
Hyperglycemia (High Blood Sugar)
Hyperglycemia occurs when glucose serum levels rise above the normal range. It is a hallmark of uncontrolled diabetes, but it can also occur in individuals who do not have diabetes due to stress, illness, or certain medications. Common causes of hyperglycemia include:
Diabetes: In individuals with type 1 or type 2 diabetes, hyperglycemia can result from a lack of sufficient insulin or insulin resistance.
Stress: Physical or emotional stress can trigger the release of stress hormones such as cortisol, which can raise blood glucose levels.
Illness: Infection, fever, and other illnesses can also raise blood sugar levels, especially in people with diabetes.
Medications: Certain medications, such as steroids, can cause glucose levels to rise.
Symptoms of hyperglycemia may include excessive thirst, frequent urination, fatigue, and blurred vision. Over time, untreated hyperglycemia can lead to complications such as diabetic ketoacidosis (in type 1 diabetes) or hyperosmolar hyperglycemic state (in type 2 diabetes), both of which can be life-threatening.
Hypoglycemia (Low Blood Sugar)
Hypoglycemia occurs when glucose serum levels drop below the normal range. This can happen when there is too much insulin in the body or if a person hasn’t eaten enough. Hypoglycemia can be particularly dangerous because the brain is highly dependent on glucose for energy. Symptoms of hypoglycemia can be subtle at first but can progress rapidly:
Early Symptoms: Shakiness, sweating, dizziness, irritability, and confusion.
Severe Symptoms: Loss of consciousness, seizures, and even coma.
Hypoglycemia can occur in people with diabetes, particularly those who are using insulin or certain oral medications that increase insulin production. It can also occur in people without diabetes, especially after long periods without eating or after intense physical activity.
Monitoring Glucose Serum Levels in Diabetes
For individuals with diabetes, monitoring glucose serum levels regularly is crucial for maintaining proper blood sugar control. Healthcare providers typically recommend a combination of methods to assess glucose levels:
1. Fasting Blood Glucose Test
The fasting blood glucose test is one of the simplest and most common ways to measure glucose serum levels. It is typically done in the morning after at least 8 hours of fasting. This test helps provide a baseline level of glucose in the bloodstream before any food intake.
2. Oral Glucose Tolerance Test (OGTT)
The OGTT is used to diagnose diabetes and prediabetes. It involves drinking a sugary solution and then measuring glucose serum levels at various intervals, typically at the 1-hour and 2-hour marks. The test measures how well the body processes glucose over time.
Normal OGTT results: A 2-hour glucose level of less than 140 mg/dL (7.8 mmol/L).
Prediabetes: A 2-hour glucose level between 140 and 199 mg/dL (7.8–11.0 mmol/L).
Diabetes: A 2-hour glucose level of 200 mg/dL (11.1 mmol/L) or higher.
3. Hemoglobin A1c Test
The hemoglobin A1c (HbA1c) test provides an estimate of average blood glucose levels over the past 2 to 3 months. It is a critical tool for assessing long-term glucose control in individuals with diabetes. While the HbA1c test does not provide real-time glucose serum levels, it reflects the overall trend in glucose management.
Normal range: Below 5.7% A1c.
Prediabetes: 5.7% to 6.4% A1c.
Diabetes: 6.5% or higher A1c.
4. Continuous Glucose Monitoring (CGM)
CGM devices are increasingly used by people with diabetes to provide real-time glucose measurements throughout the day and night. These devices are worn on the body and measure glucose levels in the interstitial fluid just beneath the skin. They offer a more dynamic and comprehensive picture of glucose fluctuations, including pre-meal and post-meal values.
Factors That Influence Glucose Serum Levels
Many factors can affect glucose serum levels. Understanding these factors is important for individuals with diabetes to manage their condition effectively:
Diet: The type, amount, and timing of food intake can significantly influence glucose levels. High-carbohydrate meals, especially those with simple sugars, can cause rapid spikes in blood glucose. Conversely, meals rich in fiber, protein, and healthy fats are less likely to cause sharp increases in blood sugar.
Exercise: Physical activity helps the body use glucose more efficiently and can lower blood sugar levels. However, intense exercise can lead to fluctuations in glucose, so individuals with diabetes must monitor their glucose closely during and after exercise.
Medications: Insulin and oral medications that increase insulin sensitivity or promote insulin production are crucial for managing glucose serum levels. The timing and dosage of these medications must be carefully balanced with food intake and physical activity.
Stress and Illness: Stress and illness can lead to elevated glucose levels due to the release of stress hormones like cortisol. Managing stress through relaxation techniques and seeking medical care during illness is important for maintaining stable glucose levels.
Sleep: Poor sleep can affect insulin sensitivity and glucose metabolism. Ensuring adequate and restful sleep can help improve blood sugar control.
Conclusion
Glucose serum level is a crucial marker of health, especially for individuals living with diabetes. By understanding what glucose serum level is, what constitutes normal and abnormal levels, and how various factors influence glucose levels, individuals can take proactive steps in managing their health. Regular monitoring of glucose levels through tests like fasting glucose, OGTT, HbA1c, and CGM, along with maintaining a balanced diet, regular exercise, and stress management, can help individuals achieve optimal glucose control and reduce the risk of complications.
For healthcare providers, understanding the nuances of glucose serum levels is essential in diagnosing and managing diabetes, ensuring that patients receive the best possible care tailored to their individual needs. By working closely with their healthcare team, individuals with diabetes can gain greater control over their glucose levels and lead healthier lives.
Related topics: