Could controlling blood sugar be the key to preserving cognitive function? Emerging research suggests a strong link between Type 2 Diabetes Mellitus (T2DM) and Alzheimer’s disease, reinforcing the idea that brain health and diabetes management are deeply intertwined. As evidence mounts, healthcare professionals are urged to consider cognitive decline as a critical factor in diabetes care, opening the door for innovative prevention and intervention strategies.
Unraveling the Link Between Diabetes and Alzheimer’s
Alzheimer’s disease is increasingly referred to as “Type 3 diabetes” due to its shared biological pathways with T2DM. While this classification is not official, it highlights key similarities in disease mechanisms. Individuals with T2DM are nearly twice as likely to develop Alzheimer’s, a correlation driven by factors such as insulin resistance, chronic inflammation, and vascular impairment.
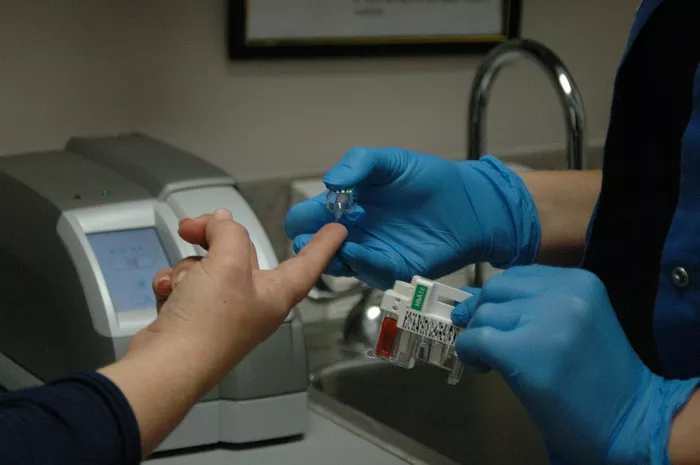
The brain depends on efficient glucose metabolism, and when insulin signaling is disrupted, cognitive function can deteriorate. According to the American Diabetes Association, nearly 60% of older adults with diabetes exhibit some degree of cognitive impairment. Moreover, chronic high blood sugar levels contribute to oxidative stress and the buildup of amyloid-beta plaques, a hallmark of Alzheimer’s pathology. Given these risks, routine cognitive screening may become an essential component of long-term diabetes management.
Biological Mechanisms Behind the Connection
The interplay between diabetes and Alzheimer’s is driven by multiple overlapping mechanisms:
Insulin Resistance and Neuronal Damage: Poor insulin regulation disrupts neuronal survival and weakens synaptic plasticity, impairing memory and cognitive function.
Inflammation and Blood-Brain Barrier Dysfunction: Diabetes-induced inflammation can compromise the blood-brain barrier, making the brain more vulnerable to toxic proteins associated with neurodegeneration.
Advanced Glycation End Products (AGEs): These harmful compounds, prevalent in diabetic patients, contribute to oxidative stress and inflammation, accelerating neuronal damage.
Mitochondrial Dysfunction and Vascular Injury: Diabetes-related mitochondrial dysfunction weakens energy production in neurons, while vascular damage restricts blood flow to the brain, further accelerating cognitive decline.
Rather than acting independently, these mechanisms create a vicious cycle, often leading to neurodegeneration that remains undiagnosed until significant symptoms emerge.
Transforming Clinical Practice: The Need for a Dual Approach
Recognizing the connection between diabetes and Alzheimer’s has significant implications for patient care. Healthcare providers must consider cognitive health as an integral part of diabetes treatment plans.
The Role of Diabetes Medications
Certain anti-diabetic drugs, such as GLP-1 receptor agonists (e.g., Trulicity and Ozempic), have shown potential neuroprotective benefits by reducing inflammation. Conversely, medications like sulfonylureas and insulin therapy, which increase the risk of hypoglycemia, have been linked to a higher likelihood of dementia. Finding a balance between glycemic control and cognitive health is essential for long-term patient well-being.
Additionally, incorporating cognitive assessment tools such as the Mini-Mental State Examination (MMSE) or Montreal Cognitive Assessment (MoCA) into routine diabetes check-ups may aid in early detection and intervention.
Prevention Strategies: Reducing Risk Through Lifestyle and Education
Preventing Alzheimer’s in diabetic patients requires a proactive approach that includes:
Lifestyle Modifications: A Mediterranean-style diet, regular physical activity, and smoking cessation have been shown to lower the risk of both diabetes and cognitive decline.
Patient Education and Support Networks: Encouraging awareness about the dual risks of diabetes and dementia can improve adherence to treatment plans. Platforms like HealingWell provide valuable community support for patients managing both conditions.
Biomarker Monitoring: Emerging biomarkers, such as phosphorylated tau and neurofilament light chain (NfL), offer promising avenues for early Alzheimer’s detection in high-risk individuals. Integrating these biomarkers into patient care may enable more personalized treatment strategies.
Conclusion
As research into Alzheimer’s and diabetes continues to evolve, the connection between the two conditions is becoming impossible to ignore. Cognitive health should be a core focus of diabetes management rather than an afterthought. Through early intervention, personalized care strategies, and a holistic approach to treatment, healthcare providers can play a crucial role in reducing the devastating impact of both diseases.
Related topics:
Link Between New-Onset Type 2 Diabetes and Obesity-Related Cancer Risk Explored
Can Diabetics Safely Enjoy Ice Cream? Here’s What Experts Recommend
Antibiotic Use in Infancy May Elevate Diabetes Risk, New Research Suggests