Managing diabetes effectively requires a thorough understanding of blood glucose levels, how they fluctuate throughout the day, and what constitutes a normal diabetic reading. Blood sugar levels play a crucial role in maintaining overall health, and staying within the recommended range helps prevent complications such as nerve damage, kidney disease, and cardiovascular problems.
This article provides an in-depth look at normal blood sugar readings for diabetics, how to interpret them, and strategies for maintaining optimal glucose control.
Blood Glucose Readings: An Overview
Blood glucose, or blood sugar, is the amount of glucose present in the bloodstream. It serves as the body’s primary source of energy and is derived from the food we eat. Insulin, a hormone produced by the pancreas, helps regulate blood sugar by allowing glucose to enter cells for energy production. In diabetes, either the body does not produce enough insulin (Type 1 diabetes) or cannot use insulin effectively (Type 2 diabetes), leading to elevated blood sugar levels.
Blood sugar levels are measured in milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L), depending on the country.
What Are Normal Blood Sugar Levels?
For Non-Diabetics
In individuals without diabetes, blood glucose levels typically remain within a narrow range:
Fasting (before meals): 70–99 mg/dL (3.9–5.5 mmol/L)
Postprandial (after meals, 1-2 hours): Below 140 mg/dL (7.8 mmol/L)
Random blood sugar: Below 140 mg/dL (7.8 mmol/L)
HbA1c (3-month average): Below 5.7%
These values indicate a well-regulated blood sugar system where insulin effectively manages glucose levels.
For Diabetics (Type 1 and Type 2 Diabetes)
People with diabetes need to maintain blood sugar levels within a specific range to avoid complications. While exact targets may vary depending on age, health conditions, and medical history, the general recommendations by the American Diabetes Association (ADA) are:
Fasting (before meals): 80–130 mg/dL (4.4–7.2 mmol/L)
Postprandial (after meals, 1-2 hours): Below 180 mg/dL (10.0 mmol/L)
Random blood sugar: Below 200 mg/dL (11.1 mmol/L)
HbA1c (3-month average): Below 7.0%
Maintaining these levels reduces the risk of diabetes-related complications, such as neuropathy, retinopathy, and cardiovascular disease.
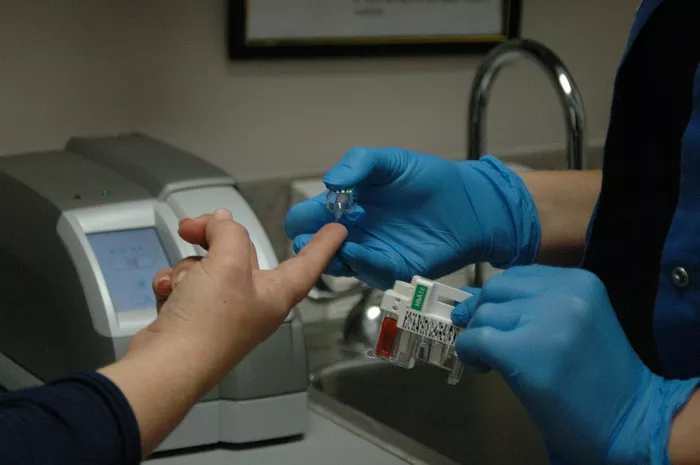
Interpreting Blood Sugar Readings
Understanding blood sugar readings is essential for managing diabetes effectively. Regular monitoring helps determine how diet, exercise, medications, and lifestyle choices impact glucose levels.
Fasting Blood Sugar (FBS)
A fasting blood sugar test is performed after at least 8 hours of fasting (typically overnight). It provides insight into baseline glucose control.
Normal: 70–99 mg/dL (3.9–5.5 mmol/L)
Prediabetes: 100–125 mg/dL (5.6–6.9 mmol/L)
Diabetes: 126 mg/dL (7.0 mmol/L) or higher on two separate tests
Postprandial Blood Sugar (PPBS)
This test is conducted 1-2 hours after a meal to assess how the body processes glucose.
Normal: Below 140 mg/dL (7.8 mmol/L)
Prediabetes: 140–199 mg/dL (7.8–11.0 mmol/L)
Diabetes: 200 mg/dL (11.1 mmol/L) or higher
HbA1c (Glycated Hemoglobin Test)
HbA1c reflects average blood glucose levels over the past 2-3 months. It helps gauge long-term diabetes control.
Normal: Below 5.7%
Prediabetes: 5.7%–6.4%
Diabetes: 6.5% or higher
Diabetics are advised to maintain an HbA1c level below 7% to minimize complications.
Factors Affecting Blood Sugar Levels
1. Diet and Nutrition
Carbohydrates have the most significant impact on blood sugar levels. Choosing complex carbohydrates such as whole grains, legumes, and vegetables can help stabilize glucose levels. High-glycemic foods, such as white bread and sugary snacks, cause rapid blood sugar spikes.
2. Physical Activity
Exercise improves insulin sensitivity and lowers blood glucose levels. Moderate-intensity activities such as brisk walking, swimming, and cycling help regulate blood sugar, while excessive exercise without adequate food intake can lead to hypoglycemia (low blood sugar).
3. Medications
Diabetics often require medications such as metformin, insulin, or other glucose-lowering drugs. Proper adherence to prescribed medications is crucial for maintaining stable blood sugar.
4. Stress and Hormones
Stress triggers the release of hormones such as cortisol and adrenaline, which can increase blood sugar levels. Stress management techniques such as meditation, deep breathing, and yoga can help regulate glucose.
5. Sleep Patterns
Poor sleep quality affects insulin sensitivity, leading to increased blood sugar levels. Maintaining a consistent sleep schedule and ensuring 7-9 hours of rest each night is essential for blood sugar control.
6. Hydration Levels
Dehydration can lead to higher blood sugar concentrations. Drinking adequate water helps the kidneys flush out excess glucose through urine.
Complications of Uncontrolled Blood Sugar
Failure to maintain blood glucose within target ranges increases the risk of diabetes-related complications, including:
Neuropathy (nerve damage): Causing numbness, tingling, and pain in extremities.
Nephropathy (kidney disease): Leading to kidney failure in severe cases.
Retinopathy (eye disease): Increasing the risk of blindness.
Cardiovascular disease: Raising the likelihood of heart attacks and strokes.
Diabetic ketoacidosis (DKA): A life-threatening condition in Type 1 diabetics caused by excessive ketone buildup.
Regular monitoring and lifestyle adjustments can significantly reduce these risks.
Tips for Maintaining Healthy Blood Sugar Levels
Follow a Balanced Diet – Prioritize fiber-rich foods, lean proteins, and healthy fats.
Monitor Carbohydrate Intake – Opt for low-glycemic carbs and practice portion control.
Engage in Regular Exercise – Aim for at least 150 minutes of moderate exercise per week.
Take Medications as Prescribed – Follow your doctor’s instructions to avoid fluctuations.
Manage Stress Effectively – Practice mindfulness, deep breathing, or engage in relaxing hobbies.
Get Enough Sleep – Maintain a consistent sleep schedule for better glucose control.
Stay Hydrated – Drink plenty of water to support glucose regulation.
Regular Blood Sugar Monitoring – Keep track of blood sugar trends to adjust diet and lifestyle accordingly.
Final Thoughts
Understanding normal diabetic readings is essential for managing blood sugar effectively and reducing the risk of complications. While diabetes requires consistent monitoring, proper lifestyle adjustments, medication adherence, and a proactive approach to health can help maintain stable glucose levels. By staying within recommended blood sugar ranges, individuals with diabetes can lead healthy, active lives while minimizing long-term health risks.
Regular check-ups with a healthcare provider are crucial for personalized guidance and adjustments to diabetes management strategies.
Related topics:
What Should Your Blood Sugar Be Before Bed?