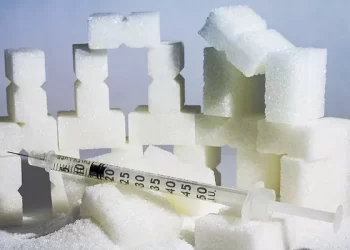
Blood glucose, also referred to as blood sugar, is the primary source of energy for the body. It comes from the food we consume and is regulated by the hormone insulin, which is produced by the pancreas. When we eat, carbohydrates are broken down into glucose, and insulin helps the cells absorb this glucose to use it for energy. However, when the body cannot regulate blood glucose levels properly, it can lead to high blood glucose, also known as hyperglycemia.
Hyperglycemia is a common issue for individuals with diabetes, but it can also occur in people without diabetes under certain conditions. Understanding what constitutes a high glucose level, how to monitor it, and when it becomes a concern are essential components of managing diabetes or preventing it from developing.
In this article, we will explore what glucose levels are considered high, the causes of high blood glucose, how it is measured, and the implications for health. We will also discuss the importance of blood glucose monitoring in managing high blood glucose and preventing complications, as well as how to respond if you experience high glucose levels.
The Importance of Blood Glucose Regulation
Before diving into what is considered a high blood glucose level, it’s crucial to understand why blood glucose regulation is so important.
Blood glucose is vital for the body’s energy, but it needs to be kept within a certain range to avoid health complications. If blood glucose is too low, a condition called hypoglycemia can occur, leading to symptoms such as dizziness, confusion, and even loss of consciousness. Conversely, if blood glucose levels are too high, it can lead to hyperglycemia, which over time can cause serious health problems, including nerve damage, kidney disease, cardiovascular disease, and diabetic retinopathy (damage to the eyes).
The body has a system in place to regulate blood glucose levels, but this system can become impaired, especially in individuals with diabetes. In people with type 1 diabetes, the pancreas cannot produce insulin, while in type 2 diabetes, the body either does not produce enough insulin or becomes resistant to it. This impaired insulin function means that glucose levels can become too high, leading to the development of hyperglycemia.
In addition to diabetes, high blood glucose levels can occur for other reasons, such as stress, illness, or the consumption of large amounts of food, especially carbohydrates. Monitoring blood glucose levels is crucial in these cases to avoid potentially dangerous outcomes.
Blood Glucose Levels: What Is Considered High?
Blood glucose levels are typically measured in milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L). The target range for blood glucose levels varies depending on factors such as whether a person has diabetes, their age, and any underlying health conditions.
For a person without diabetes, normal fasting blood glucose levels typically range between 70 to 99 mg/dL (3.9 to 5.5 mmol/L), and post-meal (after two hours) blood glucose levels should be less than 140 mg/dL (7.8 mmol/L). However, when blood glucose levels rise above these ranges, they are considered high and may indicate the presence of diabetes or prediabetes.
High Blood Glucose Levels for Non-Diabetics
In individuals without diabetes, blood glucose levels higher than the normal range may indicate a condition called prediabetes, where blood glucose levels are elevated but not high enough to be diagnosed as diabetes.
Fasting blood glucose between 100 and 125 mg/dL (5.6 to 6.9 mmol/L) is considered elevated and may indicate prediabetes.
Postprandial blood glucose (after eating) between 140 and 199 mg/dL (7.8 to 11.0 mmol/L) suggests impaired glucose tolerance, which is another indicator of prediabetes.
If a person’s blood glucose levels are consistently higher than these ranges, it can progress into type 2 diabetes. Therefore, monitoring blood glucose levels in these individuals is important to detect any early signs of diabetes and prevent its progression.
High Blood Glucose Levels for Diabetics
For individuals who have already been diagnosed with diabetes, the target blood glucose levels are generally higher than those for non-diabetics. However, it’s still important to manage blood glucose within a safe range to avoid complications. In people with diabetes, high blood glucose levels are typically defined as:
Fasting blood glucose levels greater than 130 mg/dL (7.2 mmol/L) are considered too high and may require intervention.
Postprandial blood glucose levels greater than 180 mg/dL (10.0 mmol/L) are also considered elevated and may require adjustments to medication or lifestyle changes.
It’s important to note that these target ranges may vary depending on individual factors such as age, comorbidities, and personal health goals. The goal of blood glucose management in people with diabetes is to keep blood glucose levels as close to normal as possible without increasing the risk of hypoglycemia (low blood sugar).
Hyperglycemia in Diabetics: When Should You Be Concerned?
For people with diabetes, blood glucose levels that are consistently above the target range can be considered hyperglycemia, and they should be addressed promptly to avoid further complications. However, not all high blood glucose levels require emergency intervention. There are specific thresholds that signal when medical attention may be necessary.
Mild Hyperglycemia: This occurs when blood glucose levels are slightly higher than the target range but are not dangerously elevated. For example, blood glucose levels between 180 and 250 mg/dL (10.0 to 13.9 mmol/L) may indicate mild hyperglycemia. In most cases, this can be managed with lifestyle changes, additional insulin, or other medications.
Moderate to Severe Hyperglycemia: Blood glucose levels above 250 mg/dL (13.9 mmol/L) can be considered moderate to severe hyperglycemia. At this level, individuals may begin to experience symptoms such as increased thirst, frequent urination, fatigue, and blurred vision. This requires more immediate action, such as adjusting medications, increasing insulin dosage, or seeking medical advice.
Very High Blood Glucose (Diabetic Ketoacidosis or Hyperosmolar Syndrome): Extremely high blood glucose levels (over 600 mg/dL or 33.3 mmol/L) can lead to serious medical emergencies such as diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS). Both conditions are life-threatening and require immediate medical intervention. DKA typically occurs in people with type 1 diabetes and is marked by high blood glucose, dehydration, and ketone buildup in the blood. HHS is more common in type 2 diabetes and is characterized by extreme high blood glucose without significant ketone production, but it can lead to severe dehydration and organ failure.
Causes of High Blood Glucose
High blood glucose can occur for several reasons. In individuals with diabetes, the most common causes of high blood glucose include:
Insulin Resistance: In type 2 diabetes, the body’s cells do not respond effectively to insulin, meaning that glucose cannot enter cells as efficiently. This results in elevated blood glucose levels.
Inadequate Insulin Production: In type 1 diabetes, the pancreas fails to produce insulin, and individuals rely on insulin injections or an insulin pump to regulate blood glucose. If the insulin dose is too low, blood glucose levels can rise.
Dietary Choices: Consuming large amounts of carbohydrates or sugary foods can cause blood glucose to spike, especially in individuals with diabetes who are not able to regulate glucose properly.
Stress: Stress hormones, such as cortisol, can cause an increase in blood glucose levels by promoting glucose production in the liver and reducing the body’s sensitivity to insulin.
Illness or Infection: When the body is fighting an illness or infection, stress hormones are released, and this can lead to elevated blood glucose levels. Infections can also make it more difficult for the body to use insulin properly.
Lack of Physical Activity: Physical activity helps the body use glucose for energy and improve insulin sensitivity. A sedentary lifestyle can lead to elevated blood glucose levels over time.
Medications: Certain medications, including corticosteroids, can raise blood glucose levels. Individuals taking these medications should closely monitor their blood glucose.
Alcohol: While moderate alcohol consumption can have a stabilizing effect on blood glucose, excessive drinking can cause blood sugar to rise or fall unpredictably.
Dehydration: When the body is dehydrated, blood glucose becomes more concentrated in the bloodstream, leading to higher readings.
The Importance of Monitoring Blood Glucose Levels
For individuals with diabetes, regular blood glucose monitoring is essential to detect hyperglycemia early and take the necessary actions to bring levels back into the target range. Monitoring helps individuals understand how their diet, physical activity, medications, and stress levels affect their blood glucose levels and enables them to make adjustments to maintain optimal health.
Common methods of blood glucose monitoring include:
Home Blood Glucose Meters: These devices allow individuals to test their blood glucose levels at home using a small drop of blood. Regular self-monitoring provides immediate feedback on how well blood glucose is being managed.
Continuous Glucose Monitoring (CGM): CGM systems provide real-time data on blood glucose levels throughout the day and night. These systems are often used by people with type 1 diabetes or those with poorly controlled type 2 diabetes.
Managing High Blood Glucose
If blood glucose levels are high, it’s important to take appropriate actions to bring them back into the target range. Strategies for managing high blood glucose include:
Adjusting Insulin: If you are using insulin, you may need to adjust the dosage. This can be done based on the recommendations of your healthcare provider or based on your blood glucose readings.
Physical Activity: Exercise helps lower blood glucose by allowing the muscles to use glucose for energy. Light exercise, such as walking, can be effective in reducing blood sugar levels.
Hydration: Drinking water can help flush excess glucose out of the bloodstream through urine, helping to lower blood glucose levels.
Dietary Adjustments: Reducing carbohydrate intake and consuming balanced meals can help stabilize blood sugar levels. It’s important to monitor portion sizes and avoid foods that cause significant blood sugar spikes.
Medications: Oral medications or injectable drugs like GLP-1 receptor agonists or SGLT2 inhibitors may be prescribed to help regulate blood sugar levels.
Stress Management: Since stress can elevate blood glucose, engaging in stress-reducing activities such as meditation, deep breathing, or yoga may help lower blood sugar levels.
Conclusion
High blood glucose, or hyperglycemia, is a significant concern for individuals with diabetes and can be an early indicator of underlying issues in those at risk of developing diabetes. It is essential to understand what constitutes high blood glucose, how to monitor it effectively, and when it becomes a cause for concern.
By regularly monitoring blood glucose levels and implementing appropriate strategies to manage high blood sugar, individuals can reduce their risk of developing complications related to diabetes, such as cardiovascular disease, kidney damage, and nerve problems. Whether through medication, lifestyle changes, or dietary adjustments, effective blood glucose management is key to maintaining optimal health and well-being for those with diabetes. If blood glucose levels are persistently high, it is crucial to seek professional medical advice to address the underlying causes and adjust treatment plans accordingly.
Related topics:
What is the Main Disadvantage of Using a Glucometer?