Alzheimer’s disease has long been linked to protein clumps in the brain, but growing evidence suggests that factors beyond amyloid plaques and tau tangles may play a significant role in the development of dementia. Recent studies have started to focus on diabetes and viral infections, such as herpes, as potential contributors to the disease, challenging the long-standing amyloid hypothesis.
The amyloid hypothesis, which posits that the accumulation of amyloid plaques in the brain triggers cognitive decline, has dominated Alzheimer’s research for over a century. However, new findings are casting doubt on the extent to which amyloid plaques alone are responsible for dementia symptoms. Some individuals with amyloid plaques and tau tangles do not exhibit the characteristic symptoms of Alzheimer’s, suggesting that other factors may be at play.
Investigative journalist Charles Piller, in his book Doctored: Fraud, Arrogance, and Tragedy in the Quest to Cure Alzheimer’s, raises concerns over the amyloid hypothesis, especially after a 2006 study, a cornerstone of amyloid research, was retracted due to doctored images. While Piller acknowledges that amyloid may still play a role in Alzheimer’s, he suggests that other mechanisms warrant greater attention.
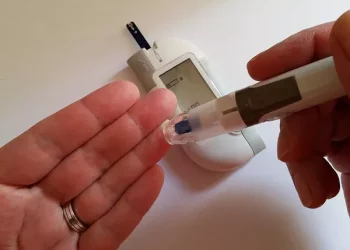
One promising avenue of research involves GLP-1 agonists, such as semaglutide, commonly used in weight-loss drugs like Ozempic and Wegovy. These drugs mimic a hormone that regulates insulin and blood sugar and have shown potential in improving brain function. Notably, people with type 2 diabetes are more than 50% more likely to develop Alzheimer’s, leading scientists to explore the connection between insulin resistance in the brain and the onset of dementia.
Professor Daniel Drucker from the University of Toronto has conducted studies highlighting the neuroprotective benefits of GLP-1 drugs. These include improved blood flow, reduced brain inflammation, enhanced communication between brain cells, and strengthened the blood-brain barrier. While the full impact on cognitive decline remains uncertain, ongoing clinical trials offer hope for new treatment options.
Another intriguing possibility is the role of dormant infections, particularly herpes simplex virus type 1 (HSV-1), in triggering Alzheimer’s. Research led by Ruth Itzhaki of the University of Manchester suggests that HSV-1, which can remain latent in the body for years, may reactivate in the brain due to factors like stress, fever, or brain injury. This reactivation can lead to inflammation and damage to brain cells, potentially accelerating the progression of dementia.
Itzhaki’s team first proposed the link between HSV-1 and Alzheimer’s in 1991, and growing evidence now supports this theory. The virus appears to be present in a significant portion of elderly brains, and repeated reactivations could contribute to the development of dementia over time. Additionally, head injuries, such as those sustained in contact sports like rugby, have been shown to increase the risk of developing dementia, further complicating the picture.
While research continues to explore these new potential causes of dementia, understanding risk factors such as diabetes, viral infections, and head trauma could offer valuable insights into prevention and treatment. As the search for a cure progresses, scientists stress the importance of managing these risk factors to reduce the overall impact of dementia on aging populations.
Related topics:
Can Diabetics Safely Enjoy Ice Cream? Here’s What Experts Recommend
Antibiotic Use in Infancy May Elevate Diabetes Risk, New Research Suggests
Wearable Technology Boosts Exercise Adherence for Type 2 Diabetes Patients