Monitoring blood sugar levels is a critical aspect of managing diabetes, and one of the key times to pay attention to these levels is at bedtime. Blood sugar levels can fluctuate throughout the day due to factors such as food intake, physical activity, stress, and medication use. Understanding what your blood sugar level should be at bedtime can help you avoid potential complications, ensure better overnight blood sugar control, and contribute to long-term diabetes management.
In this article, we will delve into the ideal blood sugar level at bedtime, how it varies for different individuals, and factors that influence nighttime blood sugar. We will also explore the consequences of uncontrolled blood sugar at night, ways to monitor blood sugar effectively before bed, and strategies to maintain healthy levels. By understanding these aspects, individuals with diabetes can take proactive steps to optimize their health and prevent overnight blood sugar fluctuations.
The Importance of Monitoring Blood Sugar at Bedtime
Monitoring blood sugar levels before bed is important for several reasons. Throughout the night, the body undergoes various physiological processes, including fasting, hormone fluctuations, and a decrease in physical activity. These changes can cause blood sugar to either rise or fall, sometimes unpredictably, especially for individuals with diabetes. Maintaining blood sugar within a healthy range at bedtime helps reduce the risk of complications like hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar) during the night.
For people with type 1 and type 2 diabetes, bedtime blood sugar levels are particularly important for preventing dangerous fluctuations during sleep. Inadequate blood sugar control at night can lead to problems such as:
Nocturnal hypoglycemia: A dangerous drop in blood sugar that can occur while sleeping, often due to insulin taken before bed or a mismatch in carbohydrate intake.
Dawn phenomenon: A natural early morning increase in blood sugar due to the body’s release of hormones like cortisol and growth hormone. Without proper bedtime control, this can result in elevated blood sugar levels upon waking.
Increased risk of long-term complications: Chronic blood sugar instability can contribute to the development of complications such as neuropathy, retinopathy, kidney disease, and cardiovascular issues.
With proper monitoring and management, these risks can be minimized, contributing to improved overall health and well-being.
Ideal Bedtime Blood Sugar Levels
The ideal blood sugar level at bedtime can vary depending on several factors, including the type of diabetes, individual health conditions, age, and other personalized factors. However, there are general guidelines that can serve as a useful reference for most people with diabetes.
For Adults with Type 1 and Type 2 Diabetes
For most adults with diabetes, the goal is to keep blood sugar levels within the following ranges before going to bed:
Pre-bedtime blood sugar: 90–150 mg/dL (5–8.3 mmol/L)
A bedtime blood sugar level in this range indicates a healthy balance between insulin levels, food intake, and the body’s natural metabolic processes. It is low enough to avoid nocturnal hyperglycemia and high enough to reduce the risk of hypoglycemia overnight.
Factors to Consider
While the general target range is helpful, it’s important to consider individual factors that may influence bedtime blood sugar levels:
Type of Diabetes
Type 1 Diabetes: For people with type 1 diabetes, blood sugar control can be more challenging due to the body’s inability to produce insulin. People with type 1 diabetes may require adjustments in their insulin therapy before bed to avoid overnight hypoglycemia.
Type 2 Diabetes: Individuals with type 2 diabetes may have varying degrees of insulin resistance and insulin production, and thus their blood sugar goals may differ based on their medication regimen, diet, and overall management plan.
Age
Older Adults: For older adults with diabetes, slightly higher blood sugar levels (around 120–150 mg/dL) before bed may be more appropriate due to increased sensitivity to insulin and a higher risk of hypoglycemia. Blood sugar levels may need to be more closely monitored and adjusted to avoid nocturnal lows.
Children and Adolescents: Children with diabetes may have slightly higher blood sugar targets before bed, often in the range of 100–180 mg/dL, as their bodies can be more prone to hypoglycemia due to their higher insulin sensitivity.
Blood Sugar History
If a person’s blood sugar levels have been trending high throughout the day, bedtime blood sugar might need to be slightly higher to compensate for potential drops overnight. Conversely, if blood sugar levels have been on the lower end of the spectrum, it’s important to monitor and correct for potential hypoglycemia.
Insulin and Medication Regimen
The type of insulin or oral medications being used to control diabetes can affect bedtime blood sugar targets. For example, long-acting insulins (like glargine or detemir) are typically used for basal coverage and may require more precise dosing adjustments to avoid nighttime hypoglycemia. Rapid-acting insulin and medications like sulfonylureas can also increase the risk of hypoglycemia if not properly managed before sleep.
Physical Activity
People who exercise later in the day may experience a drop in blood sugar levels after bedtime. This is especially true for those who engage in intense or endurance-based activities. Adjusting carbohydrate intake or insulin doses can help stabilize blood sugar overnight.
Dietary Considerations
The carbohydrate content of the evening meal can significantly influence bedtime blood sugar levels. Eating high-carbohydrate or sugary meals can cause blood sugar spikes before bed, while a meal that includes protein, healthy fats, and fiber can help stabilize blood sugar levels.
Why Do Blood Sugar Levels Fluctuate at Night?
Blood sugar fluctuations during the night are a normal part of the body’s physiological processes. However, for individuals with diabetes, these fluctuations can be more pronounced and require careful monitoring. Several factors contribute to changes in blood sugar levels during the night:
Hormonal Changes: During sleep, the body produces various hormones, including cortisol, growth hormone, and glucagon, all of which can cause blood sugar levels to rise. This is especially true in the early morning hours (the dawn phenomenon), when blood sugar can rise significantly in response to hormonal surges.
Basal Insulin and Medications: If insulin levels are too high before bed, it can lead to an overcorrection, resulting in hypoglycemia during the night. On the other hand, insufficient insulin or medication dosing may cause blood sugar to rise during sleep, which can also be problematic.
Nocturnal Hypoglycemia: Blood sugar levels may drop at night due to insulin taken earlier in the evening or from an imbalance in meal timing or carb intake. Individuals with diabetes who use insulin or certain medications may be at risk for overnight hypoglycemia if their pre-bedtime blood sugar is too low or their insulin dose is too high.
Liver Glucose Production: The liver releases glucose overnight in response to low blood sugar levels to maintain a stable energy supply. In individuals with diabetes, this process may not work as effectively, leading to high or low blood sugar levels during the night.
Risks of Abnormal Bedtime Blood Sugar Levels
Both high and low blood sugar levels at bedtime carry risks that can affect overall health and sleep quality. Let’s explore the potential consequences of uncontrolled blood sugar before bed:
1. Nocturnal Hypoglycemia
Hypoglycemia during the night is a serious risk for individuals with diabetes. Low blood sugar levels (below 70 mg/dL) can occur while asleep, leading to symptoms such as sweating, shaking, nightmares, and confusion. If left untreated, severe hypoglycemia can lead to seizures or unconsciousness. Monitoring blood sugar before bed and adjusting insulin or food intake can help prevent these dangerous events.
2. Hyperglycemia
High blood sugar levels before bed can also have negative effects. Consistently elevated blood sugar levels during the night can contribute to the development of long-term complications, such as nerve damage, kidney disease, and cardiovascular issues. Additionally, waking up with high blood sugar (often due to the dawn phenomenon) can make it more challenging to bring blood sugar back into control during the day.
3. Disrupted Sleep
Unstable blood sugar levels can lead to poor-quality sleep. Both hypoglycemia and hyperglycemia can disrupt the body’s natural sleep cycle, causing frequent awakenings and poor sleep quality. Adequate blood sugar control at bedtime helps ensure restful, uninterrupted sleep.
Strategies for Managing Bedtime Blood Sugar
To maintain optimal blood sugar levels at bedtime, it’s essential to adopt a variety of strategies that support both short-term and long-term blood sugar control. Here are some tips for managing bedtime blood sugar:
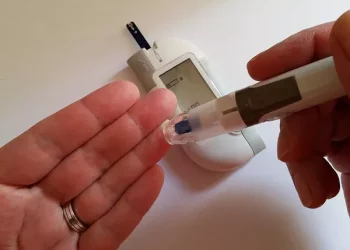
Monitor Blood Sugar Regularly: Regular blood sugar checks before bedtime can help identify patterns and make necessary adjustments to medication, diet, or lifestyle.
Adjust Insulin or Medication Doses: Work closely with your healthcare provider to adjust insulin or oral medication doses as needed to prevent nighttime blood sugar fluctuations.
Avoid Large Carbohydrate Meals Before Bed: While it’s important to eat a balanced meal, large carbohydrate-heavy meals right before bed can cause blood sugar to spike. Opt for smaller, balanced snacks that include protein and healthy fats if you need a snack before sleep.
Incorporate Low-Glycemic Foods: Choose foods with a low glycemic index for dinner and snacks. These foods help prevent rapid spikes and crashes in blood sugar levels and provide a steady source of energy.
Regular Physical Activity: Regular exercise can improve insulin sensitivity and help stabilize blood sugar levels. However, avoid intense exercise right before bed, as it may cause blood sugar to drop or spike overnight.
Manage Stress: High levels of stress can impact blood sugar control, so it’s important to practice stress management techniques, such as deep breathing, meditation, or light stretching, to promote healthy blood sugar levels.
Conclusion
Maintaining healthy blood sugar levels at bedtime is essential for overall diabetes management and preventing both short-term and long-term complications. By monitoring blood sugar before bed and adjusting insulin, diet, and lifestyle accordingly, individuals with diabetes can significantly improve their blood sugar control during the night and reduce the risk of hypoglycemia and hyperglycemia. Each person’s needs may vary, so it is important to work with a healthcare provider to develop a personalized approach to nighttime blood sugar management. By adopting these strategies, individuals can achieve better sleep, better health outcomes, and a more stable and balanced blood sugar profile.
Related topics:
Is It Worth Monitoring Blood Sugar?