Maintaining balanced blood glucose levels is a central aspect of managing diabetes and ensuring overall health. Blood glucose, or blood sugar, is a key source of energy for the body, and its levels can fluctuate throughout the day in response to a variety of factors. Understanding the different elements that influence glucose levels is essential for individuals with diabetes, as well as for those who are striving to prevent the onset of the condition. This article explores the various internal and external factors that affect glucose levels, including diet, exercise, medication, stress, sleep, and certain medical conditions.
The Role of Insulin in Glucose Regulation
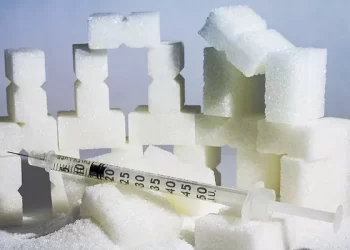
Before delving into the factors that affect glucose levels, it is important to understand the role of insulin in the body’s regulation of blood sugar. Insulin is a hormone produced by the pancreas that facilitates the entry of glucose from the bloodstream into cells for energy. In people with diabetes, the body either does not produce enough insulin or the cells become resistant to insulin, which can lead to higher-than-normal glucose levels.
For individuals with diabetes, managing blood glucose is a continuous process, as they must consider how different factors will either raise or lower their glucose levels throughout the day. Without proper regulation, persistent high glucose levels (hyperglycemia) can lead to long-term complications, while low levels (hypoglycemia) can cause immediate health risks.
Diet and Nutrition: The Most Direct Influence
One of the most significant factors influencing blood glucose levels is diet. The types of food consumed, the timing of meals, and portion sizes can have an immediate impact on blood sugar.
Carbohydrates and Glycemic Index
Carbohydrates are the most direct contributor to increased blood glucose levels. When carbohydrates are consumed, the body breaks them down into glucose, which then enters the bloodstream. Different types of carbohydrates affect blood glucose at varying rates. For example, foods with a high glycemic index (GI) — such as white bread, sugary drinks, and baked goods — cause a rapid spike in blood glucose levels. In contrast, foods with a low GI, such as whole grains, legumes, and vegetables, are digested more slowly and lead to a gradual rise in glucose.
For individuals with diabetes, understanding the glycemic index of foods can help in managing blood sugar levels. Additionally, balancing carbohydrate intake with fiber-rich foods can help moderate blood glucose levels after meals.
Portion Sizes and Meal Timing
The amount of food consumed during a meal also plays a crucial role in glucose regulation. Large portions of carbohydrates, even if they come from lower-GI foods, can still cause a significant rise in blood glucose levels. Smaller, more frequent meals throughout the day may be beneficial for some people, as they can prevent large fluctuations in blood sugar.
Meal timing is another critical consideration. For people who take insulin or other glucose-lowering medications, it is important to synchronize meal times with medication doses to ensure that glucose levels remain within a healthy range. Eating meals at irregular times or skipping meals can lead to imbalances in glucose levels, making it harder to manage the condition effectively.
Protein and Fats
While carbohydrates have the most direct impact on blood glucose, protein and fats also play a role, albeit less immediately. Protein helps to regulate glucose levels by promoting the secretion of insulin, but excessive protein intake can still have an indirect effect by triggering gluconeogenesis, the process where the liver produces glucose from non-carbohydrate sources.
Fats, especially those from healthy sources like avocados, olive oil, and nuts, can slow the absorption of glucose from carbohydrates, leading to a more gradual increase in blood sugar. However, unhealthy fats from fried foods or processed snacks can contribute to insulin resistance over time, which can worsen blood glucose control.
Physical Activity and Exercise: A Powerful Regulator
Exercise is one of the most effective ways to manage blood glucose levels. Physical activity increases the body’s sensitivity to insulin, meaning that cells are more efficient at using glucose for energy. Exercise also helps to reduce excess body fat, which is linked to insulin resistance — a condition where the body’s cells become less responsive to insulin.
Aerobic Exercise
Aerobic exercise, such as walking, running, swimming, or cycling, is particularly effective at lowering blood glucose levels by helping muscles use glucose for fuel. When people with diabetes engage in regular aerobic exercise, their bodies become better at managing glucose over time, and insulin sensitivity improves.
Resistance Training
Incorporating resistance training, such as weight lifting or bodyweight exercises, into a fitness routine also has benefits for glucose control. Muscle mass plays a significant role in glucose metabolism, and building muscle through resistance training can help to increase glucose uptake into cells. Furthermore, muscle mass helps improve overall metabolic health, leading to better long-term glucose management.
Timing of Exercise
The timing of exercise is important for blood glucose regulation. For instance, exercising after meals can help lower postprandial (after eating) blood glucose spikes. However, intense exercise can sometimes cause a temporary increase in blood sugar levels due to the release of stress hormones, such as adrenaline, which promote the release of glucose from the liver. It is important for individuals with diabetes to monitor their blood glucose before, during, and after exercise to avoid extremes of hyperglycemia or hypoglycemia.
Stress and Emotional Factors: The Impact of Hormones
Stress is another significant factor that can influence blood glucose levels, particularly for individuals with diabetes. When the body experiences stress, whether physical (due to illness or injury) or emotional (such as anxiety or depression), it releases stress hormones like cortisol and adrenaline. These hormones trigger the release of glucose from the liver, raising blood sugar levels to prepare the body for a “fight or flight” response.
Chronic stress can lead to persistently elevated glucose levels, which may worsen diabetes management. For individuals with diabetes, managing stress through relaxation techniques such as meditation, deep breathing, or yoga is important for both mental and physical health.
Sleep and Its Effect on Blood Glucose
Adequate sleep is essential for overall health, and it plays a significant role in blood glucose regulation. Poor sleep quality or insufficient sleep can negatively affect insulin sensitivity, leading to higher blood glucose levels. This is due to changes in the hormones that regulate appetite and blood sugar, such as insulin, cortisol, and ghrelin (the hunger hormone).
Sleep deprivation has been shown to increase insulin resistance, making it harder for the body to regulate glucose effectively. Additionally, poor sleep is often associated with an increased appetite for unhealthy foods, which can contribute to weight gain and further insulin resistance.
It is recommended that adults aim for 7-9 hours of sleep per night to help maintain balanced blood glucose levels. Creating a consistent sleep schedule and improving sleep hygiene (e.g., reducing screen time before bed and maintaining a quiet, dark sleep environment) can contribute to better glucose control.
Medications: Their Role and Side Effects
For many individuals with diabetes, medications are an essential component of managing blood glucose levels. There are several types of medications that can be prescribed, including oral medications, insulin injections, and newer classes of injectable drugs such as GLP-1 agonists. Each type of medication works differently to help control blood sugar.
Insulin
Insulin is the primary medication for people with type 1 diabetes and is often used by those with type 2 diabetes as well. Insulin helps regulate blood sugar by facilitating the uptake of glucose into cells. The timing and dosage of insulin are critical factors in preventing both hyperglycemia and hypoglycemia. However, insulin therapy can be complex, and if doses are not correctly adjusted for food intake, exercise, or stress levels, glucose fluctuations can occur.
Oral Medications
Oral medications for type 2 diabetes, such as metformin, sulfonylureas, and DPP-4 inhibitors, help improve the body’s ability to use insulin effectively. These medications can influence blood glucose levels by either increasing insulin sensitivity or stimulating the pancreas to produce more insulin. However, like insulin, oral medications require careful management to avoid side effects and ensure optimal glucose control.
Side Effects of Medications
Some medications can also lead to side effects that affect blood glucose levels. For example, certain steroids and antipsychotic medications can cause blood glucose levels to rise, potentially interfering with diabetes management. It is important for individuals with diabetes to work closely with their healthcare team to monitor the effects of any medications on their glucose levels and make adjustments as needed.
Medical Conditions and Hormonal Imbalances
Certain medical conditions can have a direct impact on blood glucose levels. These include:
Thyroid Disorders: Both hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid) can lead to changes in blood glucose regulation. Hypothyroidism can slow the body’s metabolism, leading to weight gain and insulin resistance, while hyperthyroidism can increase glucose production by the liver, leading to higher blood sugar levels.
Polycystic Ovary Syndrome (PCOS): PCOS is a hormonal disorder that often results in insulin resistance, making it more difficult for the body to regulate blood glucose. Women with PCOS are at increased risk of developing type 2 diabetes.
Cushing’s Syndrome: This condition, caused by excessive cortisol production, can lead to insulin resistance and higher blood glucose levels.
Infections: Illnesses, particularly infections, can elevate blood glucose levels due to the body’s stress response and the release of stress hormones. People with diabetes may need to adjust their medication or insulin doses during illness to account for these changes.
Conclusion
Blood glucose levels are influenced by a wide variety of factors, ranging from dietary choices and physical activity to stress, sleep, and medication. Understanding these factors and how they interact is crucial for individuals managing diabetes. By recognizing the complex interplay between these elements, individuals with diabetes can make more informed decisions about their lifestyle, nutrition, exercise routines, and medication, ultimately improving their ability to maintain balanced glucose levels and reduce the risk of complications.
It is important for individuals with diabetes to collaborate with healthcare providers to create personalized care plans that take into account all the factors that can affect blood glucose. With the right strategies in place, it is possible to effectively manage blood glucose levels and lead a healthy, fulfilling life.
Related topics:
What’s Normal Blood Sugar Levels for Diabetes