Diabetes is a chronic condition that affects millions of people worldwide. Proper blood sugar monitoring is crucial for managing diabetes, preventing complications, and maintaining overall health. A key part of managing blood sugar levels is understanding what constitutes a “normal” range. Blood sugar levels vary throughout the day, influenced by factors such as food intake, physical activity, and medication. Therefore, it is essential to know what range is considered healthy and how it applies to different scenarios. This article will explore the normal range for blood sugar levels, focusing on different testing methods, ideal ranges for various groups of people, and what to do when your levels fall outside the normal range.
Types of Blood Sugar Tests
Before delving into the normal blood sugar range, it’s important to understand the different types of tests used to measure blood sugar levels. Each test provides different insights into a person’s blood glucose control, helping healthcare providers track patterns and diagnose conditions.
Fasting Blood Sugar (FBS) Test: A fasting blood sugar test measures blood sugar levels after an overnight fast, typically 8–12 hours. This test is commonly used to diagnose diabetes or prediabetes. It’s one of the most effective ways to assess how the body processes glucose when not influenced by food intake.
Random Blood Sugar Test: This test measures blood sugar levels at any time of the day, regardless of when the person last ate. It’s useful for diagnosing diabetes when symptoms are present, such as excessive thirst, frequent urination, and unexplained weight loss.
Oral Glucose Tolerance Test (OGTT): The OGTT is commonly used to diagnose gestational diabetes and type 2 diabetes. After a fasting blood test, the person drinks a sugary solution, and blood sugar levels are measured at intervals over the next two hours. The response to this high dose of glucose can indicate how well the body is managing sugar.
Hemoglobin A1c (HbA1c) Test: Unlike other tests that measure short-term blood sugar fluctuations, the HbA1c test measures the average blood sugar level over the past 2–3 months. This test is crucial for diagnosing and monitoring diabetes, giving a broader picture of how well blood sugar is managed over time.
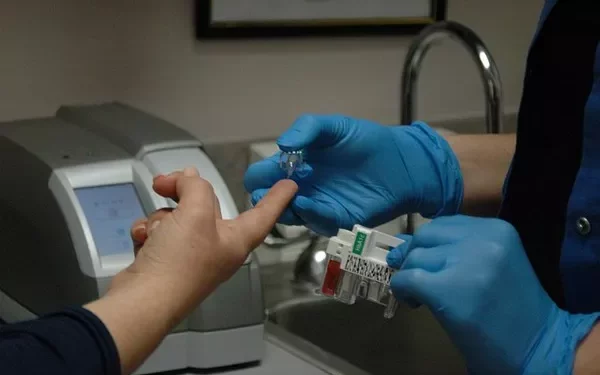
Continuous Glucose Monitoring (CGM): CGM devices provide continuous, real-time blood glucose readings throughout the day and night. The information gathered helps individuals with diabetes make informed decisions about their diet, physical activity, and insulin use.
What Is the Normal Blood Sugar Range?
Blood sugar levels can vary depending on several factors, including the time of day and the last meal consumed. Understanding the normal range for each type of test is essential for interpreting results and making decisions about health.
Fasting Blood Sugar (FBS) Test:
The fasting blood sugar test is used to measure the baseline glucose level in the blood after fasting for 8–12 hours. Here’s what the normal, prediabetic, and diabetic ranges typically look like:
Normal Range: 70–99 mg/dL (3.9–5.5 mmol/L)
Prediabetes: 100–125 mg/dL (5.6–6.9 mmol/L)
Diabetes: 126 mg/dL (7.0 mmol/L) or higher
When blood sugar levels exceed 126 mg/dL after fasting, it typically indicates that a person may have diabetes and should seek further evaluation from a healthcare provider.
Random Blood Sugar Test:
The random blood sugar test measures blood glucose at any time of the day, regardless of food intake. Here are the ranges:
Normal Range: Below 140 mg/dL (7.8 mmol/L)
Prediabetes/Impaired Glucose Tolerance: 140–199 mg/dL (7.8–11.0 mmol/L)
Diabetes: 200 mg/dL (11.1 mmol/L) or higher
A result above 200 mg/dL suggests that the person may have diabetes, especially if they are also experiencing symptoms such as excessive thirst, fatigue, and blurry vision.
Oral Glucose Tolerance Test (OGTT):
The OGTT is a more detailed test for diagnosing diabetes. After drinking a glucose solution, blood glucose levels are measured at multiple intervals. The typical ranges are:
Normal Range: Less than 140 mg/dL (7.8 mmol/L) two hours after drinking the solution
Prediabetes/Impaired Glucose Tolerance: 140–199 mg/dL (7.8–11.0 mmol/L) two hours after the test
Diabetes: 200 mg/dL (11.1 mmol/L) or higher after two hours
A reading of 200 mg/dL or higher indicates that the body cannot process glucose properly and may suggest diabetes.
Hemoglobin A1c (HbA1c) Test:
The HbA1c test provides an average blood sugar level over the past 2–3 months. This is a long-term measure of blood glucose control, often used to diagnose and monitor diabetes. The general ranges are:
Normal Range: Below 5.7%
Prediabetes: 5.7%–6.4%
Diabetes: 6.5% or higher
An HbA1c of 5.7% or above signals that the blood sugar levels have been consistently higher than normal over the past few months, indicating potential risk for diabetes.
What Affects Blood Sugar Levels?
Blood sugar levels are not constant and can be influenced by a variety of factors. These factors can make it challenging to interpret a single test result in isolation. Here are some factors that can cause fluctuations in blood glucose levels:
Diet:
The foods you eat have a direct impact on your blood sugar. Foods rich in carbohydrates, particularly refined sugars and starches, can cause a rapid rise in glucose levels. Proteins and fats tend to have a smaller impact on blood sugar, but they can also affect insulin sensitivity over time.
Physical Activity:
Exercise helps the body use glucose more efficiently. Physical activity increases insulin sensitivity, meaning the body needs less insulin to process the same amount of glucose. On the other hand, lack of exercise can lead to higher blood sugar levels.
Stress:
Stress hormones such as cortisol can cause an increase in blood sugar. This is a natural response to help the body deal with stress, but chronic stress can lead to persistent high blood sugar levels.
Medications:
Certain medications can influence blood sugar levels. For example, corticosteroids and some antipsychotic medications can raise blood sugar, while medications used to manage diabetes can lower blood sugar.
Illness:
When the body is fighting an infection, it releases stress hormones that can elevate blood sugar. Illnesses can also affect how the body responds to insulin.
Hormonal Changes:
Hormones such as insulin, cortisol, and adrenaline can affect blood sugar levels. In women, hormonal fluctuations related to menstruation, pregnancy, and menopause can cause variations in blood sugar.
What Happens When Blood Sugar Levels Are Too High or Too Low?
Maintaining a normal blood sugar range is essential for overall health. Both high and low blood sugar levels can lead to significant health issues.
Hyperglycemia (High Blood Sugar):
Chronic high blood sugar, or hyperglycemia, is a hallmark of diabetes. It can lead to long-term complications such as:
-
Damage to blood vessels, increasing the risk of heart disease, stroke, and kidney disease
-
Nerve damage (neuropathy)
-
Eye problems, including diabetic retinopathy
-
Poor wound healing and infections
Short-term hyperglycemia can cause symptoms like excessive thirst, frequent urination, fatigue, and blurred vision. Left untreated, it can lead to a life-threatening condition called diabetic ketoacidosis (DKA), especially in type 1 diabetes.
Hypoglycemia (Low Blood Sugar):
Hypoglycemia, or low blood sugar, is a condition where blood glucose levels drop below 70 mg/dL (3.9 mmol/L). Symptoms include:
-
Shakiness
-
Sweating
-
Confusion or dizziness
-
Rapid heartbeat
-
Irritability
-
Fatigue
Severe hypoglycemia can lead to unconsciousness or seizures. People with diabetes are at higher risk of hypoglycemia, particularly those who are on insulin or other medications that lower blood sugar.
How to Maintain Healthy Blood Sugar Levels
For individuals with diabetes or those at risk, maintaining healthy blood sugar levels is crucial to preventing complications. Here are several strategies for keeping blood glucose levels in check:
Eat a Balanced Diet: Focus on whole foods such as vegetables, lean proteins, whole grains, and healthy fats. Limit processed foods and those high in sugar or refined carbohydrates.
Exercise Regularly: Aim for at least 150 minutes of moderate-intensity exercise each week, such as walking, cycling, or swimming. Regular physical activity helps the body use glucose more effectively.
Monitor Blood Sugar Levels: Regular blood sugar monitoring is essential for people with diabetes. This allows individuals to make timely adjustments to their diet, exercise, and medications.
Take Medications as Prescribed: If you are prescribed medication for diabetes, it’s important to follow your healthcare provider’s instructions carefully. This includes insulin or oral medications designed to help control blood sugar levels.
Manage Stress: Practicing stress-reduction techniques such as meditation, yoga, and deep breathing exercises can help keep blood sugar levels stable.
Stay Hydrated: Drink plenty of water throughout the day to help your kidneys flush out excess sugar.
Conclusion:
Maintaining normal blood sugar levels is essential for overall health and well-being, particularly for individuals with diabetes. By understanding the normal range for blood sugar tests and monitoring your levels regularly, you can take proactive steps to prevent complications associated with high or low blood sugar. If you have concerns about your blood sugar levels or diabetes management, it’s always a good idea to consult a healthcare provider for personalized advice and guidance.
Related topics:
What’s the Ideal Glucose Levels for Diabetes Management