Gestational diabetes is a pregnancy complication that necessitates careful management to safeguard both the mother and the developing fetus. Affecting up to 10% of pregnancies in the U.S., this condition can result in serious short- and long-term complications if not properly managed. Healthcare professionals must prioritize timely diagnosis and comprehensive care to navigate this challenge successfully.
Identifying Risk Factors and Diagnostic Protocols
Understanding the risk factors and diagnostic methods for gestational diabetes is essential for effective management.
Key Risk Factors:The likelihood of developing gestational diabetes increases in women with a family history of diabetes, obesity, prior gestational diabetes, advanced maternal age, polycystic ovary syndrome (PCOS), or those from ethnic groups predisposed to diabetes.
Screening Guidelines:The American Diabetes Association (ADA) recommends universal screening for gestational diabetes at 24-28 weeks of gestation using a 75-gram Oral Glucose Tolerance Test (OGTT). High-risk patients may require earlier screening.
Diagnostic Criteria:Gestational diabetes is diagnosed if any of the following thresholds are exceeded:
- Fasting glucose ≥92 mg/dL
- 1-hour glucose ≥180 mg/dL
- 2-hour glucose ≥153 mg/dL
Differential Diagnosis:For high-risk patients, hemoglobin A1c testing at the first prenatal visit helps rule out preexisting diabetes. Early diagnosis is critical to mitigate risks such as macrosomia, preeclampsia, and neonatal hypoglycemia.
Comprehensive Management Approaches
Managing gestational diabetes involves a multidisciplinary approach to ensure optimal maternal and fetal health.
Nutritional Adjustments:A balanced diet is central to managing gestational diabetes. Clinicians should recommend smaller, frequent meals rich in fiber, lean proteins, and healthy fats. Additionally, tracking carbohydrate intake and considering the glycemic index can help regulate blood sugar levels effectively.
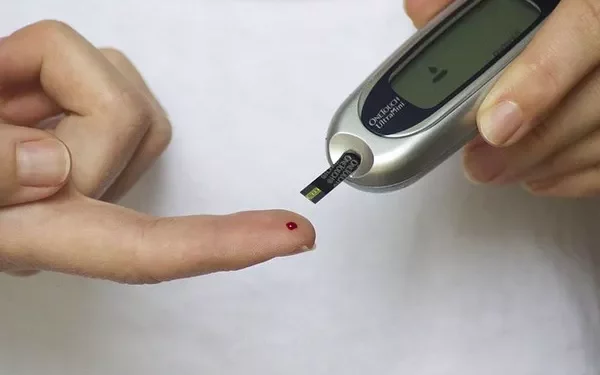
Blood Glucose Monitoring:Patients should monitor their blood glucose levels multiple times a day—before meals and postprandially. Target glucose levels may include:
- Fasting <95 mg/dL
- 1-hour post-meal <140 mg/dL
- 2-hour post-meal <120 mg/dL
Physical Activity:Moderate physical activity, such as walking or prenatal yoga, can enhance insulin sensitivity and contribute to blood sugar regulation.
Pharmacological Interventions:If lifestyle modifications are insufficient, insulin therapy is typically the first-line treatment. Medications like Metformin or Glyburide may be considered, but they require close monitoring.
Fetal Monitoring:Routine ultrasounds are necessary to assess fetal growth and detect potential complications early on.Collaboration between dietitians, endocrinologists, and obstetricians is key to ensuring comprehensive patient care.
Postpartum Care and Long-Term Risks
The management of gestational diabetes extends beyond delivery to ensure long-term health outcomes for both mother and child.
Postpartum Monitoring:Blood sugar levels typically return to normal after delivery, but postpartum glucose testing (OGTT) 6-12 weeks post-birth is crucial to identify potential persisting diabetes or prediabetes.
Risk of Type 2 Diabetes:Women with a history of gestational diabetes face a 50-70% risk of developing type 2 diabetes within 10 years. Regular A1c testing, along with lifestyle changes, is essential to mitigate this risk.
Monitoring Infant Health:Children born to mothers with gestational diabetes are at a higher risk for obesity and metabolic syndrome later in life. Regular pediatric follow-ups and guidance on healthy eating habits can help address these concerns.
Patient Education:Clinicians should emphasize the importance of maintaining a healthy weight, engaging in regular exercise, and practicing good nutrition to reduce the likelihood of gestational diabetes recurring in future pregnancies.
Conclusion
The management of gestational diabetes is an ongoing process, requiring a tailored approach, early diagnosis, and continuous support. By focusing on patient education and fostering a collaborative care environment, clinicians can significantly improve health outcomes for both mothers and their children. Empowering patients with the right knowledge ensures that both mother and baby thrive, reducing the risks associated with this prevalent pregnancy complication.
Related topics:
52-year-old Woman’s Walk for Blood Sugar Ends in Amputation.