Diabetes is a pervasive chronic condition affecting over 38 million Americans, with its impact extending beyond physical health to mental well-being. Effective management is crucial for improving health outcomes and maintaining quality of life. Dr. Emily Schroeder, an endocrinologist, recently discussed the complexities of diabetes, offering insights on prevention, treatment, and mental health challenges associated with the disease.
Understanding Diabetes
Diabetes is a metabolic disorder where the body struggles to process food for energy, leading to elevated blood sugar levels. There are three primary types of diabetes:
Type 1 Diabetes: An autoimmune condition where the body’s immune system destroys the insulin-producing cells in the pancreas.
Type 2 Diabetes: Characterized by insulin resistance, where the body does not effectively use insulin, leading to high blood sugar levels.
Gestational Diabetes: Occurs during pregnancy, resulting from hormonal changes that make the body less responsive to insulin. This type typically resolves after childbirth.
Risk Factors for Diabetes
While genetic predisposition plays a role in both type 1 and type 2 diabetes, lifestyle factors significantly affect the development of type 2 diabetes. Family history is a notable risk factor, as are environmental and behavioral influences such as being overweight, leading a sedentary lifestyle, or consuming an unhealthy diet. Women who experience gestational diabetes and their children are at heightened risk of developing type 2 diabetes later in life.
Preventing Diabetes through Lifestyle Changes
For those diagnosed with prediabetes, where blood sugar levels are elevated but not yet in the diabetic range, lifestyle modifications are key in preventing full-blown diabetes. Recommendations include:
Achieving a Healthy Weight: Losing just 5-7% of body weight has been shown to significantly reduce the risk of progressing to diabetes.
Balanced Diet: Consuming a diet rich in whole foods—fruits, vegetables, whole grains, nuts, and unprocessed proteins—while cutting back on refined carbs and processed foods.
Increasing Physical Activity: Regular exercise, aiming for at least 150 minutes of moderate activity per week, can help control blood sugar and improve overall health.
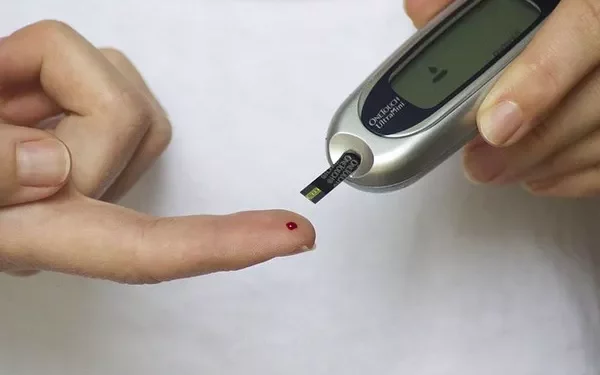
Monitoring Key Health Indicators: Keeping track of A1C levels, blood pressure, and cholesterol can aid in early detection and prevention.
These strategies can vary depending on individual health conditions, so it is important to consult with a healthcare provider to tailor interventions that are safe and effective.
Reversing Type 2 Diabetes
In some cases, individuals with type 2 diabetes can reverse the condition by losing weight and making dietary changes that restore insulin sensitivity. However, this is not always achievable for everyone. For those who cannot reverse the condition, medications are available to manage blood sugar, such as insulin, drugs that enhance insulin usage, and others that slow digestion or reduce appetite.
Unlike type 2 diabetes, type 1 diabetes is not reversible with lifestyle changes. However, advancements in treatment have been made. The U.S. Food and Drug Administration recently approved islet cell transplantation for individuals with type 1 diabetes who experience severe hypoglycemia despite intensive management. This procedure involves transplanting healthy insulin-producing cells from a donor pancreas into the recipient’s liver, where they can produce insulin.
Additionally, a medication called TZIELD® (teplizumab-mzwv) is now approved for children aged 8 and older to delay the onset of type 1 diabetes by preserving pancreatic function.
The Intersection of Diabetes and Mental Health
Living with diabetes can take a toll on mental health. The constant management required—monitoring blood sugar, adhering to medications, and maintaining a strict lifestyle—can lead to diabetes burnout. This condition is characterized by feelings of disengagement, hopelessness, and difficulty maintaining self-care routines. People experiencing burnout may also neglect medical appointments or adopt unhealthy eating habits.
Mental health struggles such as depression and anxiety are common in individuals with diabetes. Recognizing the signs of burnout is crucial, and stress-management strategies such as meditation, yoga, and time in nature can provide relief. If symptoms persist, it’s important to seek support from a healthcare provider to develop a manageable treatment plan.
Support and Resources for Diabetes Care
Managing diabetes effectively requires a team approach, including education, support, and guidance from healthcare professionals. At Parkview Diabetes Care Services, a dedicated team of diabetes educators, dietitians, and specialists provides personalized care to help individuals navigate their condition. For more information about programs and support resources, call Parkview Diabetes Care Services at 260-373-4280.
Conclusion
Managing diabetes is a lifelong commitment that involves addressing both physical and mental health needs. With the right lifestyle changes, medical interventions, and support, individuals with diabetes can lead healthy and fulfilling lives.
Related topics:
Study Links Ozempic to Increased Risk of Optic Nerve Damage
Hydration’s Role in Blood Sugar Management: How Drinking Water Impacts Diabetes