Lifestyle Modifications: The Cornerstone
Dietary Changes: A balanced diet is essential. This involves reducing the intake of simple carbohydrates like refined sugars and white bread. Instead, an emphasis is placed on complex carbohydrates such as whole grains, which have a lower glycemic index and cause a slower rise in blood glucose levels. Increasing the consumption of fiber-rich foods like fruits, vegetables, and legumes is also beneficial. Fiber helps in delaying the absorption of glucose and improves glycemic control. For example, a diet rich in oats and barley can help regulate blood sugar. Moreover, controlling portion sizes is crucial to manage calorie intake and maintain a healthy body weight.
Physical Activity: Regular exercise is highly recommended. It helps in increasing insulin sensitivity. Aerobic exercises like walking, jogging, cycling, or swimming for at least 150 minutes per week can significantly improve glycemic control. Resistance training, such as lifting weights or using resistance bands, is also beneficial as it helps in building muscle mass. Muscle tissue is more sensitive to insulin than fat tissue, and thus, an increase in muscle mass can enhance glucose uptake. Even simple activities like taking the stairs instead of the elevator or walking short distances instead of using a vehicle can contribute to the overall physical activity level.
Weight Management: Maintaining a healthy weight is a key aspect. For overweight or obese patients, even a modest weight loss of 5 – 10% of body weight can have a significant impact on blood glucose levels. This can be achieved through a combination of dietary changes and increased physical activity. Weight loss reduces insulin resistance and allows the body to use insulin more effectively. For instance, a patient who loses weight may find that their blood sugar levels become more stable and may require less medication to control their diabetes.
Oral Antidiabetic Agents: Pharmacological Options
Metformin: It is often considered the first line pharmacological treatment for type 2 diabetes. Metformin works by reducing hepatic glucose production. It inhibits the enzyme gluconeogenesis in the liver, thereby decreasing the amount of glucose released into the bloodstream. It also improves insulin sensitivity in peripheral tissues such as muscle and fat. One of the advantages of metformin is its relatively low risk of causing hypoglycemia. Additionally, it may have beneficial effects on cardiovascular risk factors. For example, it can help in reducing LDL cholesterol levels. However, it may cause side effects such as gastrointestinal upset, including nausea, vomiting, and diarrhea. But these side effects can often be managed by starting with a low dose and gradually increasing it.
Sulfonylureas: These drugs stimulate the pancreas to secrete more insulin. They act on the beta cells of the pancreas to enhance insulin release. For example, glipizide and glyburide are commonly used sulfonylureas. They can effectively lower blood glucose levels, especially in patients with residual pancreatic beta cell function. However, the main drawback is the risk of hypoglycemia. Patients taking sulfonylureas need to be careful about their meal timings and monitor their blood sugar levels closely to avoid hypoglycemic episodes. Moreover, they may cause weight gain over time, which can have a negative impact on overall diabetes management.
DPP – 4 Inhibitors: Dipeptidyl peptidase – 4 inhibitors work by increasing the levels of incretin hormones. These hormones, such as glucagon – like peptide – 1 (GLP – 1), are secreted in response to food intake and have several beneficial effects. They stimulate insulin secretion, suppress glucagon release, and slow down gastric emptying. Sitagliptin and saxagliptin are examples of DPP – 4 inhibitors. They have a relatively low risk of hypoglycemia and are generally well – tolerated. They can be used as an alternative to metformin in patients who cannot tolerate metformin or in combination with metformin for better glycemic control. However, long – term studies are still ongoing to fully assess their cardiovascular and other potential side effects.
GLP – 1 Receptor Agonists: A Promising Class
Mechanism of Action: GLP – 1 receptor agonists mimic the action of the natural incretin hormone GLP – 1. They bind to GLP – 1 receptors in the pancreas, gut, and brain. By doing so, they stimulate insulin secretion in a glucose – dependent manner, which means that insulin is secreted only when blood glucose levels are elevated. They also suppress glucagon secretion, which further helps in reducing blood glucose levels. Additionally, they slow down gastric emptying, leading to a feeling of satiety and potentially aiding in weight loss.
Examples and Benefits: Exenatide and liraglutide are well – known GLP – 1 receptor agonists. These drugs have shown significant improvements in glycemic control. In addition to their glucose – lowering effects, they can lead to weight loss, which is beneficial for many patients with type 2 diabetes who are overweight or obese. They also have a relatively low risk of hypoglycemia. Some studies have suggested potential cardiovascular benefits, such as a reduction in the risk of major adverse cardiovascular events. However, they are injectable medications, which may be a deterrent for some patients. Side effects can include nausea, vomiting, and diarrhea, especially in the initial stages of treatment, but these usually subside over time.
SGLT2 Inhibitors: Novel Therapeutic Agents
How They Work: Sodium – glucose cotransporter 2 (SGLT2) inhibitors work by blocking the reabsorption of glucose in the kidneys. Normally, the kidneys reabsorb most of the filtered glucose back into the bloodstream. SGLT2 inhibitors prevent this reabsorption, leading to increased urinary excretion of glucose. This results in a reduction in blood glucose levels. Canagliflozin and dapagliflozin are examples of SGLT2 inhibitors.
Advantages and Considerations: One of the major advantages of SGLT2 inhibitors is their potential to cause weight loss and blood pressure reduction. They have also been shown to have beneficial effects on cardiovascular and renal outcomes. For example, they may reduce the risk of heart failure hospitalization and slow down the progression of diabetic kidney disease. However, they can increase the risk of urinary tract infections and genital mycotic infections due to the increased glucose in the urine. There have also been concerns about a rare but serious side effect called diabetic ketoacidosis, although the incidence is relatively low.
Insulin Therapy: When and How
Indications for Starting Insulin: Insulin therapy is usually considered when other oral antidiabetic agents and lifestyle modifications fail to achieve adequate glycemic control. This may be the case in patients with very high blood glucose levels at diagnosis, those who have had type 2 diabetes for a long time and have progressive beta cell failure, or patients with significant comorbidities that require rapid and effective glycemic control. For example, a patient with type 2 diabetes and concurrent acute coronary syndrome may need to start insulin therapy to quickly bring down their blood sugar levels.
Types of Insulin and Regimens: There are different types of insulin, including short – acting, intermediate – acting, and long – acting insulins. A common regimen may start with basal insulin, which provides a background level of insulin throughout the day and night. For example, insulin glargine is a long – acting insulin. As the disease progresses, a combination of basal and prandial insulin (insulin taken before meals to cover the postprandial glucose rise) may be required. However, insulin therapy requires careful monitoring of blood glucose levels, as the risk of hypoglycemia is relatively high. Patient education on insulin injection techniques, dose adjustment, and recognition and treatment of hypoglycemia is essential.
Patient Education and Self – Management: Empowering the Patient
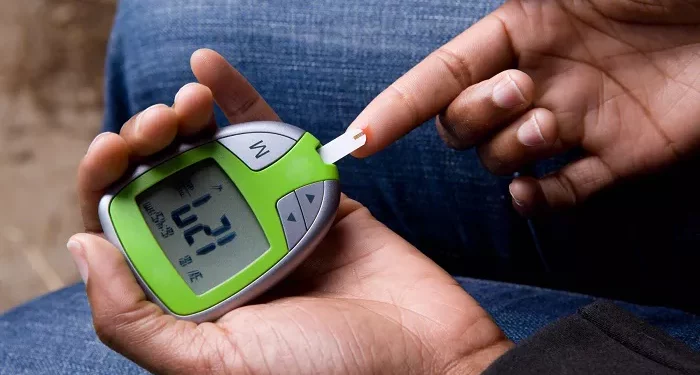
Blood Glucose Monitoring: Patients need to be educated on how to monitor their blood glucose levels regularly. This helps in understanding the effects of diet, exercise, and medications on blood sugar. They should know when and how to use a glucometer, and how to record and interpret the results. For example, a patient may need to monitor their blood sugar before and after meals, as well as at bedtime, to adjust their treatment plan accordingly.
Medication Adherence: Understanding the importance of taking medications as prescribed is crucial. Patients should be aware of the proper dosage, timing, and potential side effects of their medications. They should also know what to do if they miss a dose. For example, if a patient taking metformin misses a dose, they may need to take it as soon as they remember, unless it is close to the next scheduled dose.
Recognition and Management of Hypoglycemia and Hyperglycemia: Patients must be able to recognize the symptoms of hypoglycemia, such as sweating, trembling, confusion, and weakness. They should know how to treat it promptly, usually by consuming a fast – acting source of glucose like a glucose tablet or fruit juice. Similarly, they should be aware of the symptoms of hyperglycemia, such as excessive thirst, frequent urination, and blurred vision, and understand the importance of seeking medical attention if blood sugar levels remain high for an extended period.
Conclusion
The first line treatment for type 2 diabetes is a multifaceted approach. Lifestyle modifications should always be emphasized and implemented. Depending on the patient’s specific characteristics, one or more pharmacological agents may be added. Patient education and self – management are integral parts of successful diabetes management. A personalized treatment plan that takes into account the patient’s individual needs and goals is essential to achieve optimal glycemic control and prevent the long – term complications associated with type 2 diabetes. Healthcare providers need to have a comprehensive understanding of all available treatment options and work closely with patients to make informed decisions about the most appropriate first line treatment strategy.
Related topics