Metformin: The First-Line Defense
Metformin is often considered the cornerstone of type 2 diabetes treatment. It belongs to the biguanide class of drugs and has been in use for decades. Here’s why it’s so popular:
Mechanism of Action: Metformin works primarily by reducing the amount of glucose produced by the liver. It also improves the body’s sensitivity to insulin, allowing cells to take up glucose more effectively from the bloodstream. For instance, when a person eats a meal, instead of the liver releasing excessive amounts of glucose, metformin helps keep those levels in check, preventing postprandial blood sugar spikes.
Benefits: One of the major advantages of metformin is its ability to aid in weight loss or at least prevent further weight gain, which is beneficial as many patients with type 2 diabetes struggle with obesity. It has also been shown to have a positive impact on lipid profiles, potentially reducing the risk of heart disease. Additionally, metformin is relatively inexpensive compared to many other diabetes medications, making it accessible to a large number of patients.
Side Effects: While generally well-tolerated, metformin can cause some gastrointestinal issues like nausea, diarrhea, and abdominal discomfort, especially when starting the medication or increasing the dose. These side effects usually subside over time. In rare cases, lactic acidosis, a serious condition where there is a buildup of lactic acid in the body, can occur. However, this is extremely uncommon and more likely in patients with kidney or liver problems.
Sulfonylureas: Stimulating Insulin Release
How They Work: These medications work by binding to specific receptors on pancreatic beta cells, which stimulates the release of insulin. Essentially, they coax the pancreas to produce more insulin than it normally would, thereby lowering blood glucose levels. For example, if a patient’s pancreas isn’t secreting enough insulin after a meal, sulfonylureas can prompt it to release a sufficient amount to handle the glucose load.
Advantages: Sulfonylureas are highly effective at quickly reducing blood sugar levels. They are available in both short-acting and long-acting formulations, allowing for flexibility in dosing depending on the patient’s needs. For patients with severely elevated fasting blood glucose levels, long-acting sulfonylureas can provide consistent control throughout the day.
Disadvantages: The main drawback is the risk of hypoglycemia (low blood sugar). Since they directly stimulate insulin release, if a patient takes too much, skips a meal, or exercises more than usual, their blood sugar can drop dangerously low. Weight gain is also a common side effect, which can be counterproductive as excess weight often exacerbates insulin resistance in type 2 diabetes patients.
DPP-4 Inhibitors: A Gentle Approach to Blood Sugar Regulation
Mode of Action: DPP-4 is an enzyme that breaks down incretin hormones in the body. Incretins are responsible for stimulating insulin release after a meal and suppressing glucagon, a hormone that raises blood sugar. DPP-4 inhibitors block this enzyme, allowing incretin hormones to remain active longer, which in turn leads to increased insulin secretion and decreased glucagon production, maintaining more stable blood sugar levels.
Benefits: These drugs are generally well-tolerated with a low risk of hypoglycemia, making them a good option for patients who are prone to low blood sugar with other medications. They also don’t cause significant weight gain or loss, which is appealing for those concerned about body weight. Moreover, many DPP-4 inhibitors can be taken once daily, enhancing patient compliance.
Drawbacks: Some patients may experience mild side effects like upper respiratory tract infections, headache, or nasopharyngitis. Additionally, while effective for many, they may not provide sufficient blood sugar control on their own for patients with very high glucose levels, often necessitating combination therapy with other medications.
GLP-1 Receptor Agonists: Beyond Blood Sugar Control
Functionality: GLP-1 is a hormone that is released in response to food intake. GLP-1 receptor agonists mimic the action of this hormone, stimulating insulin secretion when blood sugar is high, suppressing glucagon release, and slowing down gastric emptying. By slowing digestion, they prevent rapid spikes in blood sugar after a meal. For example, when a patient consumes a carbohydrate-rich meal, the drug ensures that the glucose is absorbed more gradually into the bloodstream.
Advantages: In addition to excellent blood sugar control, GLP-1 receptor agonists have been shown to promote weight loss, sometimes significant amounts. This dual benefit of glycemic control and weight reduction is highly valuable for obese patients with type 2 diabetes. They also have a beneficial effect on cardiovascular health, reducing the risk of major cardiovascular events like heart attacks and strokes.
Side Effects: Common side effects include nausea, vomiting, and diarrhea, especially when starting the medication. However, these usually diminish over time as the body adjusts. There’s also a rare risk of pancreatitis and thyroid C-cell tumors, although the evidence for the latter is still being studied, and the overall occurrence is extremely low.
SGLT2 Inhibitors: A Novel Way to Excrete Glucose
How They Operate: Normally, the kidneys reabsorb glucose back into the bloodstream. SGLT2 inhibitors work by blocking the SGLT2 transporters in the kidneys, preventing glucose reabsorption. As a result, excess glucose is excreted in the urine, thereby lowering blood sugar levels. This process is independent of insulin, which is particularly beneficial for patients with advanced insulin resistance.
Benefits: Besides reducing blood glucose, SGLT2 inhibitors have shown remarkable cardioprotective and renoprotective effects. They can lower blood pressure, reduce the risk of heart failure hospitalization, and slow the progression of kidney disease in patients with diabetes. Some studies have also suggested a potential reduction in mortality rates associated with their use.
Downsides: The most noticeable side effect is an increased risk of urinary tract infections and genital mycotic infections due to the higher glucose levels in the urine, providing a favorable environment for bacteria and fungi. Additionally, there have been rare cases of ketoacidosis reported, although this is not common and often occurs in specific clinical scenarios.
Insulin Therapy: When All Else Falls Short
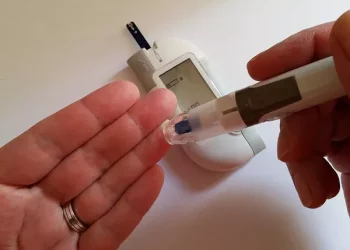
Indications for Use: Insulin is typically introduced when other medications fail to achieve adequate blood sugar control. This could be due to worsening pancreatic function over time, where the pancreas produces less and less insulin. It’s also used in cases of severe hyperglycemia or during periods of physiological stress like illness or surgery when blood sugar levels become extremely difficult to manage with oral drugs alone.
Types of Insulin: There are various types of insulin, including rapid-acting, short-acting, intermediate-acting, and long-acting formulations. Rapid-acting insulin starts working within minutes and peaks in about an hour, mimicking the body’s natural insulin response to a meal. Long-acting insulin, on the other hand, provides a steady basal level of insulin throughout the day, keeping fasting blood sugar levels stable.
Challenges: Insulin therapy requires careful dosing and monitoring as incorrect administration can lead to hypoglycemia. It also often involves injections, which can be a psychological barrier for some patients. Additionally, weight gain is a common side effect, similar to what’s seen with sulfonylureas, which may further complicate diabetes management in overweight or obese patients.
Conclusion
Related topics