Monitoring blood glucose is a cornerstone of managing diabetes. For individuals living with diabetes, understanding blood glucose readings can be the difference between effective disease management and complications. The importance of blood glucose control cannot be overstated, as it directly impacts long-term health outcomes. Knowing what your blood glucose number means is essential for maintaining a balanced lifestyle and ensuring that the body functions optimally.
This article delves into the significance of blood glucose readings, how they are interpreted, what different readings indicate, and how they inform decisions about diabetes management. We will explore how factors like time of day, food intake, physical activity, and medication use can influence glucose numbers, and provide insights on how to maintain your glucose levels within a healthy range.
The Basics of Blood Glucose
Blood glucose, also known as blood sugar, refers to the amount of glucose circulating in the bloodstream. Glucose is a vital source of energy for the body’s cells and is primarily derived from food, especially carbohydrates. After food is consumed, the digestive system breaks it down into glucose, which then enters the bloodstream. The body’s pancreas releases insulin, a hormone that helps regulate blood glucose levels by allowing glucose to enter cells for energy or storage.
In healthy individuals, blood glucose levels fluctuate throughout the day depending on factors like eating, exercise, and metabolic rate. For individuals with diabetes, however, blood glucose levels may be higher or lower than desired due to insulin resistance or insufficient insulin production. Monitoring blood glucose levels is therefore critical in preventing both short-term and long-term complications associated with diabetes.
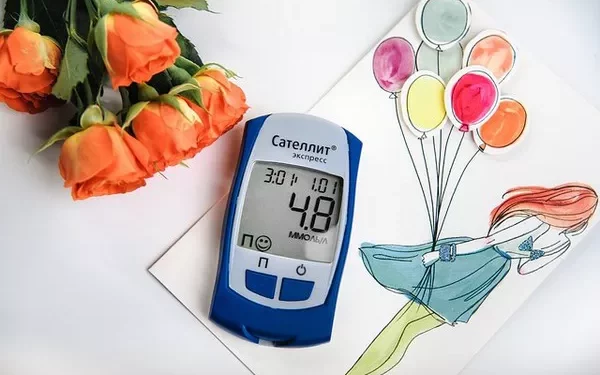
How Blood Glucose Is Measured
Blood glucose is typically measured in milligrams per deciliter (mg/dL) in the United States or millimoles per liter (mmol/L) in most other countries. The measurement can be taken at any time of day and is generally categorized into different types based on the timing of the test:
Fasting Blood Glucose (FBG): A fasting blood glucose test is performed after an overnight fast of at least 8 hours. This provides an accurate reading of the body’s baseline glucose level in the absence of food.
Postprandial Blood Glucose: This is measured 2 hours after eating a meal. It provides insight into how the body processes glucose after food intake.
Random Blood Glucose: This test is done at any time of the day, regardless of when the person last ate. It is useful for assessing blood glucose during different parts of the day.
Hemoglobin A1c (HbA1c): Although not a direct measure of blood glucose, HbA1c gives an average of the blood glucose level over the past 2-3 months. It is particularly helpful in assessing long-term glucose control.
Each of these methods provides valuable information about blood glucose levels, and it is important to understand how to interpret the results for better management of diabetes.
Interpreting Blood Glucose Numbers
Blood glucose readings are usually classified into several categories depending on whether they are taken during fasting, after meals, or randomly. The ranges for normal, prediabetic, and diabetic blood glucose levels are as follows:
1. Fasting Blood Glucose Levels
Normal: A fasting blood glucose level between 70-99 mg/dL (3.9-5.5 mmol/L) is considered normal.
Prediabetes: A fasting blood glucose level between 100-125 mg/dL (5.6-6.9 mmol/L) indicates prediabetes, a condition where blood glucose levels are higher than normal but not yet high enough to be diagnosed as diabetes.
Diabetes: A fasting blood glucose level of 126 mg/dL (7.0 mmol/L) or higher on two separate occasions is diagnostic of diabetes.
2. Postprandial Blood Glucose Levels
Normal: A postprandial blood glucose level less than 140 mg/dL (7.8 mmol/L) two hours after eating is considered normal.
Prediabetes: A blood glucose level between 140-199 mg/dL (7.8-11.0 mmol/L) two hours after eating suggests impaired glucose tolerance, which is a prediabetic condition.
Diabetes: A postprandial blood glucose level of 200 mg/dL (11.1 mmol/L) or higher, two hours after a meal, is consistent with a diagnosis of diabetes.
3. Random Blood Glucose Levels
Normal: A random blood glucose level below 140 mg/dL (7.8 mmol/L) is generally considered normal.
Prediabetes/Diabetes: A random blood glucose level above 200 mg/dL (11.1 mmol/L), along with symptoms of diabetes (such as increased thirst, frequent urination, or unexplained weight loss), may suggest diabetes.
4. Hemoglobin A1c (HbA1c)
The HbA1c test reflects the average blood glucose level over the past 2-3 months. It provides a longer-term view of blood glucose control.
Normal: An HbA1c level below 5.7% is considered normal.
Prediabetes: An HbA1c level between 5.7% and 6.4% indicates prediabetes.
Diabetes: An HbA1c level of 6.5% or higher on two separate occasions is diagnostic of diabetes.
Understanding Blood Glucose Fluctuations
Blood glucose levels are never static; they fluctuate throughout the day based on various factors. These fluctuations are influenced by a combination of dietary choices, physical activity, medication use, stress, and other physiological factors.
1. Effect of Food on Blood Glucose Levels
The food you eat plays a major role in determining your blood glucose level. Carbohydrates, in particular, have the most significant impact, as they are broken down into glucose and absorbed into the bloodstream. Foods with a high glycemic index (GI) cause rapid spikes in blood glucose, while foods with a low GI release glucose more slowly.
Simple Carbohydrates: Foods such as white bread, sugary snacks, and sweetened beverages are digested quickly, leading to sharp increases in blood glucose.
Complex Carbohydrates: Whole grains, legumes, and vegetables are digested more slowly, providing a steadier release of glucose into the bloodstream.
For individuals with diabetes, it is important to balance carbohydrate intake and pair carbs with protein and healthy fats to minimize blood glucose spikes. Additionally, understanding portion sizes is key to preventing excessive increases in blood glucose levels.
2. Physical Activity and Exercise
Exercise is a natural way to help lower blood glucose levels. During physical activity, muscles use glucose for energy, which can lead to a reduction in blood glucose. Regular exercise, particularly aerobic activities such as walking, swimming, or cycling, can improve insulin sensitivity, helping the body use glucose more efficiently.
However, the relationship between exercise and blood glucose is complex. Intense or prolonged exercise can sometimes lead to a temporary rise in blood glucose levels due to the release of stress hormones like cortisol and adrenaline. It is essential to monitor blood glucose before, during, and after exercise to adjust insulin or carbohydrate intake as needed.
3. Medication and Insulin
For individuals with diabetes, medications or insulin therapy are often required to help regulate blood glucose levels. The timing, dosage, and type of medication can influence blood glucose readings. Insulin, for example, is designed to help lower blood glucose levels, while medications like glucagon-like peptide-1 (GLP-1) agonists or sodium-glucose cotransporter 2 (SGLT2) inhibitors have other mechanisms of action.
It is important to understand how different medications affect blood glucose levels. For instance, too much insulin can lead to hypoglycemia (low blood glucose), while too little can lead to hyperglycemia (high blood glucose). Regular monitoring helps ensure that medications are working effectively and that blood glucose stays within target ranges.
4. Stress and Emotional Health
Stress can have a profound impact on blood glucose levels. When the body is stressed, it releases hormones such as cortisol and adrenaline, which can cause an increase in blood glucose levels. This is especially problematic for people with diabetes, as their bodies may already have difficulty regulating glucose. Learning to manage stress through relaxation techniques, physical activity, or mindfulness can help maintain more stable blood glucose levels.
5. Illness and Infection
Being ill can also lead to changes in blood glucose levels. Infections, fevers, and inflammation trigger the release of stress hormones, which can elevate blood glucose levels. Furthermore, some illnesses may reduce the appetite, which can affect food intake and insulin requirements. During periods of illness, it is crucial to monitor blood glucose more frequently and adjust diabetes management accordingly.
What Do High or Low Glucose Numbers Mean?
1. High Blood Glucose (Hyperglycemia)
Consistently high blood glucose levels, or hyperglycemia, are a hallmark of poorly controlled diabetes. Chronic hyperglycemia can lead to a variety of complications, including:
Increased risk of cardiovascular disease: Chronic high blood glucose can damage blood vessels and increase the risk of heart disease, stroke, and other vascular problems.
Nerve damage (neuropathy): High glucose levels can cause nerve damage, leading to symptoms like tingling, numbness, and pain, particularly in the feet and hands.
Kidney damage (nephropathy): The kidneys can be damaged by prolonged hyperglycemia, leading to diabetic nephropathy, which may progress to kidney failure.
Vision problems: High blood glucose can damage the blood vessels in the eyes, leading to diabetic retinopathy and even blindness if not managed.
Signs of hyperglycemia include increased thirst, frequent urination, fatigue, and blurred vision. If blood glucose levels rise significantly, it may lead to diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS), which are medical emergencies.
2. Low Blood Glucose (Hypoglycemia)
Hypoglycemia occurs when blood glucose levels drop too low, typically below 70 mg/dL (3.9 mmol/L). This can result from taking too much insulin, skipping meals, or excessive physical activity without adequate carbohydrate intake. Symptoms of hypoglycemia include shaking, sweating, dizziness, confusion, and even loss of consciousness.
Severe hypoglycemia requires immediate treatment, often with glucose tablets, sugary drinks, or intravenous glucose if the person cannot swallow. Regular monitoring and adjusting insulin or medication doses can help prevent hypoglycemia.
Conclusion
Understanding your blood glucose numbers is crucial for managing diabetes effectively. By regularly monitoring your glucose levels and interpreting the results accurately, you can make informed decisions about diet, exercise, medication, and overall diabetes management. Blood glucose readings provide valuable insights into how your body is responding to the demands of daily life and can help prevent both short-term fluctuations and long-term complications.
Ultimately, successful diabetes management requires an individualized approach, working closely with healthcare providers to optimize treatment and lifestyle choices. By learning what your blood glucose numbers mean, you are taking an important step toward achieving better control over your health and preventing the complications of diabetes.
Related topics:
How to Get a Free Blood Glucose Monitor