Blood sugar monitoring is one of the cornerstones of diabetes management. Keeping track of your blood glucose (sugar) levels allows individuals with diabetes to manage their condition effectively and avoid complications. Understanding what constitutes a “good” average blood sugar level is essential for people with diabetes, as it influences treatment decisions, lifestyle choices, and long-term health outcomes. This article explores what a good average blood sugar level is, how to monitor it effectively, and how to maintain healthy blood sugar levels for optimal diabetes management.
The Importance of Blood Sugar Monitoring in Diabetes
Diabetes is a chronic condition that affects the body’s ability to process glucose, a primary source of energy. The hormone insulin, which is produced by the pancreas, helps regulate blood sugar levels by facilitating the movement of glucose from the bloodstream into the body’s cells. In individuals with diabetes, either insufficient insulin production or insulin resistance causes blood glucose levels to rise, leading to hyperglycemia (high blood sugar). Over time, poorly controlled blood sugar levels can result in complications such as heart disease, kidney failure, nerve damage, and vision problems.
Blood sugar monitoring is an essential tool in managing diabetes. By regularly checking blood glucose levels, individuals can assess how well their diabetes management plan is working and make necessary adjustments to their diet, exercise, medication, or insulin regimen. Regular monitoring helps prevent extreme blood sugar fluctuations, reduce the risk of complications, and maintain an overall sense of well-being.
What is Blood Sugar?
Blood sugar refers to the amount of glucose present in the blood. Glucose comes from the food we eat, especially carbohydrates, which are broken down into glucose during digestion. Blood sugar is essential for energy, but maintaining it within a specific range is crucial for optimal health, particularly for individuals with diabetes.
Blood sugar levels can vary throughout the day depending on a variety of factors, such as:
What you eat: Meals and snacks, especially those high in carbohydrates, can cause an increase in blood sugar.
How active you are: Physical activity can help lower blood sugar by allowing muscles to use glucose for energy.
Medications: Insulin and other diabetes medications help control blood glucose levels.
Time of day: Blood sugar levels tend to be lower in the morning before eating, and they can rise after meals.
Average Blood Sugar Levels for Diabetics
For people with diabetes, understanding what constitutes a “good” average blood sugar is important for preventing complications. Blood sugar levels are usually measured in milligrams per deciliter (mg/dL) in the United States or in millimoles per liter (mmol/L) in other countries. While blood glucose levels can vary from person to person, the American Diabetes Association (ADA) provides general guidelines for blood sugar targets, which are often used as a reference for assessing the average range.
Normal Blood Sugar Levels
Before discussing what a good average blood sugar is for those with diabetes, it’s helpful to understand what normal blood sugar levels look like for individuals without diabetes. According to the ADA:
Fasting blood sugar (measured after at least 8 hours of fasting): 70-99 mg/dL (3.9-5.5 mmol/L)
Postprandial blood sugar (measured 2 hours after eating): Less than 140 mg/dL (7.8 mmol/L)
Random blood sugar: Less than 200 mg/dL (11.1 mmol/L)
For those without diabetes, blood sugar levels are typically well-regulated by the body’s natural insulin response.
Blood Sugar Targets for People with Diabetes
For people with diabetes, the ADA recommends slightly higher target blood sugar levels to accommodate the body’s difficulty in managing glucose. However, it is important to note that individual goals can vary depending on factors such as age, duration of diabetes, overall health, and whether complications are present. Here are the general blood sugar targets for adults with diabetes:
Fasting blood sugar: 80-130 mg/dL (4.4-7.2 mmol/L)
Postprandial blood sugar (2 hours after meals): Less than 180 mg/dL (10.0 mmol/L)
A1C level: Less than 7%
A1C: A Key Measure of Average Blood Sugar
The A1C test, also called the glycated hemoglobin test, is one of the most important tools used to assess average blood sugar levels over a period of 2-3 months. It provides a long-term picture of how well blood glucose levels have been managed. Unlike daily blood sugar tests, which provide a snapshot of glucose levels at a specific moment, the A1C test reflects average blood sugar levels over time.
The A1C level is measured as a percentage. The higher the percentage, the higher the average blood sugar. A1C is typically used as an indicator for overall diabetes management, as it helps track whether treatment is working and whether the risk of complications is increasing.
Normal A1C: Less than 5.7%
Pre-diabetes: A1C between 5.7% and 6.4%
Diabetes: A1C of 6.5% or higher
For most individuals with diabetes, the goal is to keep the A1C level below 7%. However, some individuals may aim for a lower target, especially if they are younger, otherwise healthy, and at low risk for hypoglycemia (low blood sugar). On the other hand, older adults or those with more advanced diabetes may have a higher target to reduce the risk of low blood sugar.
Factors That Influence Blood Sugar Levels
Blood sugar levels can fluctuate throughout the day based on a variety of factors. Managing blood glucose is not only about what you eat but also about understanding how other factors interact with your blood sugar. These factors include:
1. Diet and Carbohydrate Intake
Carbohydrates are the primary macronutrient that affects blood sugar levels. Foods like bread, pasta, rice, and fruits are broken down into glucose during digestion, leading to an increase in blood sugar. The glycemic index (GI) of a food can also influence how quickly blood sugar rises. Low-GI foods, such as whole grains and vegetables, tend to cause slower increases in blood sugar, while high-GI foods, such as sugary snacks, lead to rapid spikes.
Managing carbohydrate intake is essential for blood sugar control, as consuming too many carbs can result in hyperglycemia. People with diabetes are often advised to monitor their carbohydrate intake and spread it out throughout the day to maintain stable blood sugar levels.
2. Exercise and Physical Activity
Physical activity helps lower blood sugar by increasing insulin sensitivity and allowing muscles to use glucose for energy. Regular exercise, especially aerobic activities such as walking, running, or cycling, can help prevent high blood sugar (hyperglycemia) and improve overall blood glucose control. However, it’s important to monitor blood sugar levels before, during, and after exercise to avoid low blood sugar (hypoglycemia), especially if insulin or medications are being used.
3. Medications and Insulin
For people with diabetes, medications such as insulin or oral hypoglycemic agents are necessary to help manage blood sugar levels. The timing, dose, and type of medication can significantly impact how blood glucose levels fluctuate throughout the day. Insulin therapy, for example, helps reduce high blood sugar, while medications like metformin improve insulin sensitivity. It’s crucial to work closely with a healthcare provider to adjust medications and insulin regimens as needed.
4. Stress
Stress activates the body’s “fight-or-flight” response, which leads to the release of stress hormones such as cortisol. These hormones can cause blood sugar levels to rise, making stress management an important part of diabetes care. Stress-reducing techniques such as yoga, meditation, and deep breathing exercises can help mitigate the impact of stress on blood glucose levels.
5. Sleep
Lack of sleep can contribute to insulin resistance and make it more difficult to maintain stable blood sugar levels. Poor sleep may cause blood sugar to rise, especially in individuals with diabetes. Ensuring adequate rest and managing sleep disorders can contribute to better blood glucose control.
How to Monitor Blood Sugar Effectively
Regular blood sugar monitoring is essential for individuals with diabetes to understand how their diet, lifestyle, and medications affect their blood glucose levels. Monitoring blood glucose involves testing blood sugar levels using a glucometer or continuous glucose monitoring (CGM) system.
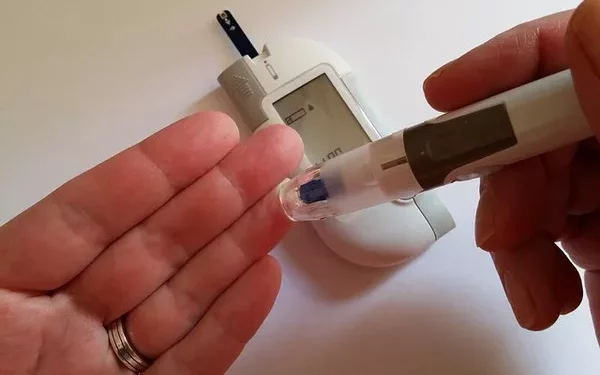
1. Using a Glucometer
A glucometer is a handheld device that measures blood sugar levels from a small drop of blood, usually obtained by pricking a fingertip. The blood sugar level is displayed in mg/dL (or mmol/L), and results typically take just a few seconds. Most people with diabetes are encouraged to test their blood sugar at different times during the day, including before and after meals, to assess how food, exercise, and medications impact their blood glucose levels.
2. Continuous Glucose Monitoring (CGM)
A CGM system is a device that provides continuous readings of blood sugar levels throughout the day and night. It consists of a small sensor that is placed under the skin to measure glucose in the interstitial fluid. CGM systems can help identify trends in blood sugar levels and offer real-time alerts if blood glucose is too high or low. This system is especially useful for people with type 1 diabetes or those who experience frequent blood sugar fluctuations.
Maintaining a Healthy Blood Sugar Average
Achieving and maintaining a good average blood sugar requires a holistic approach to diabetes management. Here are some strategies for keeping blood glucose levels within target range:
Eat a balanced diet: Focus on whole foods, high-fiber vegetables, lean proteins, and healthy fats. Limit processed foods and sugars.
Exercise regularly: Aim for at least 150 minutes of moderate-intensity exercise each week.
Take medications as prescribed: Follow your healthcare provider’s instructions regarding insulin and other medications.
Monitor blood sugar regularly: Check your blood glucose at key times to understand how food, activity, and medications affect your levels.
Manage stress: Incorporate relaxation techniques into your daily routine to manage stress.
Get enough sleep: Aim for 7-9 hours of sleep per night to support overall health and blood sugar control.
Conclusion
A good average for blood sugar varies by individual, but generally, people with diabetes should aim for a fasting blood sugar of 80-130 mg/dL (4.4-7.2 mmol/L), a postprandial blood sugar of less than 180 mg/dL (10.0 mmol/L), and an A1C level below 7%. Achieving these targets involves regular monitoring, medication adherence, a balanced diet, and an active lifestyle. By maintaining consistent blood sugar levels, individuals with diabetes can reduce the risk of complications and improve their quality of life.
Related topics:
What is Normal Reading for Sugar Level