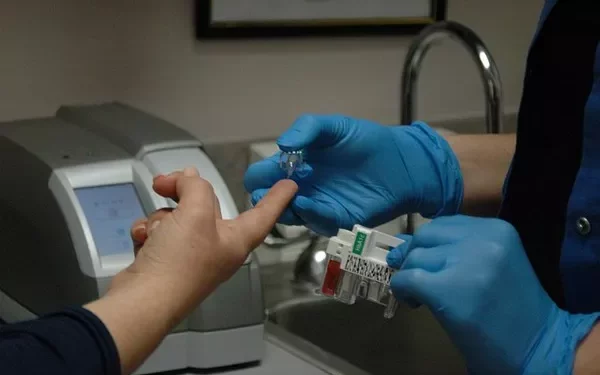
Blood sugar monitoring is an essential aspect of diabetes management, enabling individuals with diabetes to track their glucose levels and adjust their treatment plans accordingly. Traditionally, this process involved fingerstick tests, where a small blood sample was taken, and glucose levels were measured using a glucose meter. However, the advent of continuous glucose monitoring (CGM) technology has introduced new options for patients seeking more convenient and continuous ways to track their blood sugar levels. Among the innovations in this area are blood sugar watches, wearable devices designed to continuously monitor blood glucose levels without the need for frequent fingersticks.
These devices, often marketed as blood sugar watches, promise to provide users with real-time data on their blood glucose levels and allow for more effective management of diabetes. But the question remains: Do blood sugar watches really work? Are they accurate, reliable, and practical enough to be a suitable alternative to traditional monitoring methods? This article will explore the technology behind blood sugar watches, evaluate their effectiveness, and discuss the pros and cons of using these devices as part of a diabetes management plan.
Understanding Continuous Glucose Monitoring (CGM) Technology
Before delving into the specific capabilities of blood sugar watches, it’s important to first understand how continuous glucose monitoring (CGM) systems work. Continuous glucose monitoring is a technology that allows for the real-time measurement of glucose levels in the interstitial fluid (the fluid between cells) rather than directly in the blood. These devices are typically composed of three key components:
Sensor: A small sensor is inserted just under the skin, typically on the abdomen or the upper arm. The sensor continuously measures glucose levels in the interstitial fluid.
Transmitter: The sensor is connected to a transmitter, which sends glucose data wirelessly to a receiver or mobile app. Some CGMs send data to a dedicated device, while others can sync directly with smartphones or smartwatches.
Receiver/Display: The receiver or display unit shows the real-time glucose data, and in some cases, provides trend graphs and alerts when glucose levels are too high or too low.
Unlike traditional fingerstick methods, CGMs provide a continuous stream of data, allowing users to track fluctuations in blood glucose levels throughout the day and night. CGMs can alert users to rapidly changing glucose levels, helping them take corrective action before glucose levels become dangerously high or low.
Blood sugar watches, which integrate CGM technology into a wearable watch-like form, are a relatively new development in diabetes management. These devices are designed to be worn like a traditional watch, offering the convenience of constant glucose monitoring while maintaining a discreet, user-friendly design.
How Blood Sugar Watches Work
Blood sugar watches, also known as wearable continuous glucose monitors, combine the functionality of CGMs with the ease and convenience of a smartwatch. These devices are typically worn on the wrist, and they continuously track glucose levels by using sensors that are either integrated into the watch itself or worn on the body in conjunction with the watch. The key to these devices lies in their ability to communicate with sensors and transmit data wirelessly to the watch for real-time display.
The primary components of blood sugar watches are similar to traditional CGMs, but the device’s design is tailored for wearability and ease of use. Here’s how they work:
Sensor Integration: Some blood sugar watches integrate the sensor directly into the watch strap, while others may require users to wear a separate sensor patch on the body. These sensors detect glucose levels in the interstitial fluid and send the data to the watch in real time.
Data Display: The watch displays glucose data on its screen, allowing users to see their blood glucose levels instantly. Some watches also feature trend lines, showing how glucose levels are rising or falling over time, which can be especially useful for tracking patterns and identifying potential issues.
Alerts and Notifications: One of the most significant advantages of blood sugar watches is their ability to alert users when glucose levels are too high or too low. These alerts are usually customizable, allowing users to set their own thresholds for when they need to take corrective action.
Mobile App Integration: Many blood sugar watches sync with a smartphone app that provides even more detailed insights into glucose trends, historical data, and recommendations for managing blood sugar levels. The apps may also allow users to share their data with healthcare providers for better management.
While blood sugar watches offer a convenient, non-invasive way to monitor glucose levels, the accuracy and reliability of these devices remain a key concern. To understand whether blood sugar watches really work, we need to evaluate their performance, compare them to traditional methods of blood sugar monitoring, and consider the benefits and limitations of using them for diabetes management.
Accuracy and Reliability of Blood Sugar Watches
One of the most critical factors in determining the effectiveness of blood sugar watches is their accuracy. For a blood sugar monitor to be considered reliable, it must provide accurate readings that are consistent with those obtained through traditional fingerstick blood glucose testing. Inaccurate readings can lead to poor decision-making, resulting in either unnecessary corrective actions (such as excessive insulin administration) or a failure to address dangerously high or low blood sugar levels.
Most blood sugar watches rely on sensors that measure glucose in the interstitial fluid rather than directly in the blood. While the glucose levels in interstitial fluid generally reflect those in the blood, there can be a delay between changes in blood glucose and changes in interstitial glucose. This delay, known as the “lag time,” can vary depending on factors such as how quickly glucose levels are changing, the location of the sensor, and the user’s individual physiology. Typically, lag times can range from a few minutes to up to 15 minutes.
In terms of overall accuracy, blood sugar watches generally perform well but are not without their limitations. According to research and clinical trials, CGM devices (and by extension, blood sugar watches) typically have a mean absolute relative difference (MARD) of about 10-15%. This means that, on average, the readings may vary by 10-15% from a traditional blood glucose meter’s results. While this level of accuracy is sufficient for many people with diabetes, it can be problematic in situations where precise blood sugar control is crucial, such as for patients using insulin pumps or those with very tight glucose control goals.
For most people, blood sugar watches provide sufficient accuracy for day-to-day monitoring. However, the FDA and other regulatory agencies have not approved blood sugar watches for use as a replacement for traditional blood glucose meters in situations where blood glucose testing is required by law, such as for making insulin dosing decisions.
Advantages of Blood Sugar Watches
Despite some of the limitations regarding accuracy, there are several key benefits to using blood sugar watches as part of diabetes management:
Continuous Monitoring: One of the most significant advantages of blood sugar watches is the ability to continuously track blood glucose levels. Traditional fingerstick testing only provides a snapshot of glucose at a particular moment in time, while CGMs provide a more comprehensive view of glucose trends. This continuous data stream can help users identify patterns, such as spikes in blood glucose after meals or drops in glucose levels during exercise or sleep.
Convenience and Comfort: Blood sugar watches are easy to wear and comfortable, making them an excellent option for individuals who want a less invasive way to monitor their blood glucose. Many users find the ease of wearing a watch much more comfortable than traditional sensors or frequent fingerstick tests, which can be painful or inconvenient.
Real-Time Alerts: Blood sugar watches provide real-time alerts for low or high blood sugar levels, helping users take corrective action immediately. These alerts can be customized based on the user’s glucose thresholds, providing a personalized approach to blood sugar management.
Trend Data: In addition to displaying real-time glucose readings, blood sugar watches often provide users with visual data trends, such as graphs showing how blood glucose is trending over time. This information can be helpful for identifying the causes of blood glucose fluctuations and making informed decisions about food, exercise, and medication.
Improved Diabetes Management: The continuous nature of monitoring with blood sugar watches can lead to better overall control of blood glucose levels. By providing more data and timely alerts, these devices can help people with diabetes make adjustments in real time, reducing the risk of both hyperglycemia and hypoglycemia.
Integration with Other Devices: Many blood sugar watches can sync with other diabetes management tools, such as insulin pumps or smartphone apps. This integration can further streamline diabetes management by providing a centralized platform for tracking glucose levels, medication, diet, and exercise.
Disadvantages of Blood Sugar Watches
While blood sugar watches offer many benefits, there are also some drawbacks and challenges associated with their use:
Cost: Blood sugar watches and continuous glucose monitoring systems can be expensive, especially when considering the costs of sensors, transmitters, and ongoing supplies. This can be a barrier to access for some individuals, particularly those without insurance coverage for these devices.
Accuracy Limitations: As previously mentioned, the accuracy of blood sugar watches can be limited compared to traditional blood glucose meters. The lag time between changes in blood glucose and changes in interstitial fluid glucose can lead to delayed alerts and inaccuracies in real-time data.
Battery Life and Maintenance: Blood sugar watches typically require regular charging, and the sensors may need to be replaced every few days or weeks. This maintenance requirement can be inconvenient and costly over time.
Calibration Needs: Some blood sugar watches require periodic calibration using a traditional blood glucose meter, which can be cumbersome and may negate the convenience factor of using a continuous monitoring system.
Limited Regulatory Approval: While blood sugar watches are often FDA-approved for general use, they are not yet considered a replacement for traditional blood glucose meters for insulin dosing decisions. As such, they may not be suitable for all individuals, particularly those who require precise insulin management.
Comfort and Fit: Depending on the design, some users may find blood sugar watches bulky or uncomfortable, especially when worn during sleep. Additionally, sensors may need to be attached to the skin in conjunction with the watch, which can be inconvenient.
Conclusion: Are Blood Sugar Watches Worth It?
Blood sugar watches are an innovative and useful tool for people with diabetes who seek continuous glucose monitoring without the invasiveness of traditional testing methods. While they are not without their limitations—such as issues with accuracy, lag time, and cost—these devices offer several key benefits, including real-time data, continuous monitoring, trend analysis, and personalized alerts. For many individuals, blood sugar watches can significantly improve diabetes management and quality of life.
However, it is important for users to understand the limitations of these devices and work closely with healthcare providers to integrate them into a broader diabetes management plan. Blood sugar watches are not a one-size-fits-all solution, and their effectiveness will vary depending on individual needs, lifestyle, and glucose control goals.
As the technology continues to evolve, we can expect blood sugar watches to become even more accurate, accessible, and user-friendly. For now, they represent an exciting advancement in diabetes care and a valuable tool for those looking for a more convenient and continuous way to monitor their glucose levels.
Related topics: