Blood glucose monitoring is a critical component of diabetes management. For individuals with diabetes, keeping blood sugar levels in check is essential to preventing both short-term complications, such as hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar), and long-term complications, including cardiovascular disease, nerve damage, and kidney problems. Blood glucose monitors (BGMs), also known as glucose meters, are indispensable tools in this process. This article provides a detailed explanation of how blood glucose monitors work, the different types available, how to use them, and how they play a vital role in managing diabetes effectively.
What is Blood Glucose Monitoring?
Blood glucose monitoring refers to the regular testing of blood sugar levels to track how they fluctuate throughout the day and how they respond to different factors, such as food intake, physical activity, medication, and stress. For individuals with diabetes, monitoring blood glucose levels is necessary to ensure that they stay within the target range recommended by healthcare providers. This helps prevent complications associated with both high and low blood sugar levels.
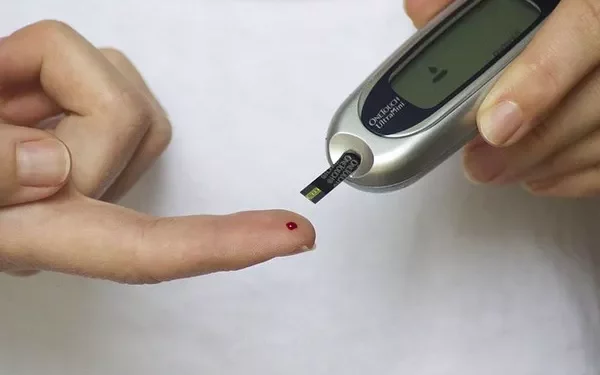
A blood glucose monitor is a device used to measure the concentration of glucose (sugar) in a sample of blood. It typically involves pricking the skin with a lancet (a small, sharp needle) to obtain a tiny blood sample, which is then placed on a test strip that interacts with the glucose in the blood. The monitor uses the chemical reaction that occurs on the strip to calculate the blood glucose level and display it on the device’s screen.
The Importance of Blood Glucose Monitoring
For individuals with diabetes, effective blood glucose monitoring is a cornerstone of disease management. Regular monitoring helps with:
Personalized Treatment Adjustments: Monitoring blood glucose levels enables individuals and their healthcare providers to adjust medication (such as insulin doses), food intake, and exercise plans based on real-time data.
Tracking Patterns: Frequent blood sugar checks allow individuals to observe patterns and trends in their glucose levels, providing valuable insight into how certain foods, activities, and medications affect their blood sugar.
Preventing Complications: Maintaining blood glucose levels within the target range reduces the risk of complications such as diabetic neuropathy, retinopathy, kidney disease, and cardiovascular disease.
Empowerment and Control: By regularly checking glucose levels, individuals can feel more in control of their diabetes, leading to better adherence to treatment plans and healthier lifestyle choices.
How Does a Blood Glucose Monitor Work?
Blood glucose monitors work through a process that involves sampling blood, applying it to a test strip, and measuring the glucose concentration in the sample. Though the specific technologies used in different devices may vary, the basic principle is similar across most monitors. Below is a breakdown of how glucose monitors function:
1. Blood Sample Collection
The process begins with obtaining a blood sample, typically through a fingerstick, although alternate sites like the forearm, thigh, or abdomen may be used in some devices. The lancet is used to make a small puncture in the skin, and the user applies a drop of blood to the test strip.
The amount of blood required for the test is usually very small—about a drop or less—and it is absorbed by the test strip. The size of the sample may vary depending on the model of the glucose meter, but modern devices require only a small amount of blood, making the process relatively painless.
2. Test Strips and Chemical Reaction
Test strips are an essential part of the blood glucose monitoring system. These strips contain chemicals that react with glucose in the blood sample. When the blood is placed on the strip, it interacts with the chemicals embedded in the strip, causing a chemical reaction. This reaction generates an electrical signal or changes in light absorbance, depending on the type of glucose meter being used.
The test strip is designed to bind to glucose molecules specifically, allowing the device to measure the amount of glucose in the blood sample accurately. Some test strips also contain an enzyme called glucose oxidase, which catalyzes a reaction between glucose and oxygen, generating a measurable current proportional to the glucose concentration.
3. Signal Processing and Measurement
Once the blood sample interacts with the test strip, the glucose monitor processes the signal generated by the chemical reaction. The method of measurement varies depending on the technology used by the meter. There are three primary types of glucose meters based on the type of sensor they use:
Electrochemical Sensors: This is the most common type of glucose meter used today. In this system, the test strip contains an enzyme, typically glucose oxidase or glucose dehydrogenase, that reacts with glucose in the blood sample. This reaction produces an electrical current. The glucose meter measures the magnitude of this current, which is directly proportional to the amount of glucose in the sample. This current is then converted into a digital readout, displaying the blood glucose level on the monitor.
Colorimetric Sensors: In colorimetric meters, the glucose test strip contains chemicals that undergo a color change when they react with glucose in the blood sample. The glucose monitor uses optical sensors to measure the intensity of the color change, which correlates with the concentration of glucose. These meters are less common today but were used in earlier models.
Optical Sensors: Optical sensors use light to detect glucose levels. The test strip may contain materials that absorb or emit light when exposed to glucose. The monitor shines light onto the test strip and measures the way light is absorbed or reflected, which allows it to determine the concentration of glucose in the sample.
4. Displaying the Results
Once the glucose meter processes the information from the test strip, it displays the result on the device’s screen. The result is typically shown in milligrams per deciliter (mg/dL) in the United States and some other countries, or in millimoles per liter (mmol/L) in countries like Canada, the UK, and Australia.
Blood glucose monitors usually display results within a few seconds to a minute, making them convenient for daily monitoring. Some advanced meters may also offer additional information, such as averages over a set period or trend graphs showing changes in glucose levels over time.
5. Alternative Site Testing (AST)
In addition to fingerstick testing, some glucose monitors allow for alternative site testing (AST), where blood samples can be taken from other parts of the body, such as the forearm, thigh, or abdomen. AST can be less painful and more convenient, but it’s important to note that blood glucose levels may differ from those measured at the fingertips, particularly after meals or during periods of rapid glucose change. Therefore, AST is usually recommended for non-urgent testing, and fingerstick testing is preferred when blood glucose levels are fluctuating rapidly or if immediate treatment decisions need to be made.
Types of Blood Glucose Monitors
There are several types of blood glucose monitors available, ranging from basic models to advanced systems that offer additional features. Below are the most common types:
1. Traditional Blood Glucose Meters (BGMs)
Traditional BGMs are the most commonly used glucose monitors. These devices require a small blood sample, typically from a fingertip, which is applied to a disposable test strip. The meter calculates the glucose level and displays the result. These meters are affordable, easy to use, and offer quick results. Most models are portable and do not require additional technology or a smartphone connection.
2. Continuous Glucose Monitors (CGMs)
Continuous glucose monitors (CGMs) are advanced devices that measure glucose levels continuously throughout the day and night. A small sensor is inserted under the skin, usually in the abdomen or arm, where it measures glucose levels in the interstitial fluid (the fluid between cells). CGMs provide real-time glucose readings, which can be monitored on a smartphone or a separate receiver.
CGMs can help individuals track their glucose levels continuously and detect trends, allowing for proactive adjustments to medication, diet, and activity. They also alert users to potential highs or lows in blood glucose levels, which can be critical for preventing hypoglycemia or hyperglycemia.
3. Smart Glucose Meters
Smart glucose meters are glucose monitoring devices that can connect to smartphones, tablets, or computers. These devices often work in conjunction with apps that allow users to log their blood glucose results, food intake, exercise, and medication use. The app can analyze trends and provide reports that can be shared with healthcare providers. Smart meters also offer the convenience of storing multiple readings and generating insights that can help individuals with diabetes optimize their management plan.
4. Non-Invasive Glucose Monitors
Non-invasive glucose monitoring is an emerging area of technology. These devices do not require blood samples but instead use sensors to measure glucose levels in the body through the skin or via other bodily fluids. While there is a lot of ongoing research into non-invasive glucose monitoring, these devices are not yet as accurate or widely available as traditional glucose meters.
Best Practices for Blood Glucose Monitoring
To ensure the accuracy of blood glucose readings, individuals should follow these best practices:
Use Clean Hands: Always wash hands thoroughly before testing to avoid contamination from food, dirt, or other substances that may interfere with the blood sample.
Correct Test Strip Handling: Handle test strips carefully to prevent contamination, as moisture, heat, or dirt can affect the accuracy of the reading.
Consistent Testing Sites: Use the same testing site consistently for accurate comparisons, especially when using alternate site testing.
Follow Manufacturer Instructions: Different meters have different operating procedures. Always follow the manufacturer’s instructions for using the device and test strips.
Conclusion
Blood glucose monitoring is a cornerstone of effective diabetes management. Blood glucose monitors allow individuals with diabetes to track their glucose levels, make informed decisions about their treatment, and avoid complications related to abnormal blood sugar levels. With various types of meters available, ranging from traditional devices to advanced continuous glucose monitors, the technology continues to evolve, offering more convenience, accuracy, and integration with other health data. Proper use of these tools helps individuals manage their condition, leading to better health outcomes and improved quality of life.
Related topics:
What is a Normal A1C Level in a Blood Test?