Managing diabetes effectively is an ongoing challenge that requires attention to several factors, including diet, exercise, medications, and most importantly, blood sugar control. Blood sugar (glucose) levels can fluctuate throughout the day, and for individuals with diabetes, maintaining these levels within a healthy range is essential to avoid complications such as nerve damage, cardiovascular disease, kidney damage, and vision problems. One of the most important tools in the management of diabetes is blood sugar monitoring, which enables individuals to track and adjust their treatment plans based on real-time glucose readings.
Blood sugar monitoring is widely recommended by healthcare providers, yet many people with diabetes still have questions about the benefits and practical use of blood glucose meters. Is it truly necessary for managing diabetes? What are the advantages of frequent monitoring? And how can it be used effectively to improve health outcomes?
In this article, we will explore the significance of blood sugar monitoring, how it works, the different types of blood glucose meters available, and the many ways it can help individuals with diabetes take control of their condition. We will also discuss the benefits of continuous monitoring and provide practical tips for integrating blood sugar checks into your daily routine.
Why Is Blood Sugar Monitoring Important for Diabetes?
Blood sugar monitoring is crucial for the management of both type 1 and type 2 diabetes. For individuals with type 1 diabetes, their pancreas produces little to no insulin, meaning they must take insulin injections or use an insulin pump to regulate blood sugar levels. For people with type 2 diabetes, the body either does not produce enough insulin or cannot effectively use the insulin it does produce. Both conditions can lead to fluctuating blood sugar levels, which can be dangerous if left unmanaged.
Understanding Blood Sugar Fluctuations
Blood glucose levels typically rise after eating and can dip after periods of fasting or exercise. For people without diabetes, the body’s natural mechanisms—primarily insulin production—help maintain blood sugar levels within a narrow range. However, for people with diabetes, these mechanisms are disrupted, which can lead to both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar).
Without effective monitoring, it can be difficult to know when blood sugar levels are too high or too low, putting individuals at risk for long-term complications. Monitoring blood sugar levels allows individuals to detect these fluctuations and take corrective actions, such as adjusting insulin doses, modifying their diet, or increasing physical activity.
How Blood Sugar Monitoring Works
Blood sugar monitoring involves measuring the concentration of glucose in the blood. There are two main methods of monitoring blood glucose: self-monitoring of blood glucose (SMBG) and continuous glucose monitoring (CGM).
Self-Monitoring of Blood Glucose (SMBG)
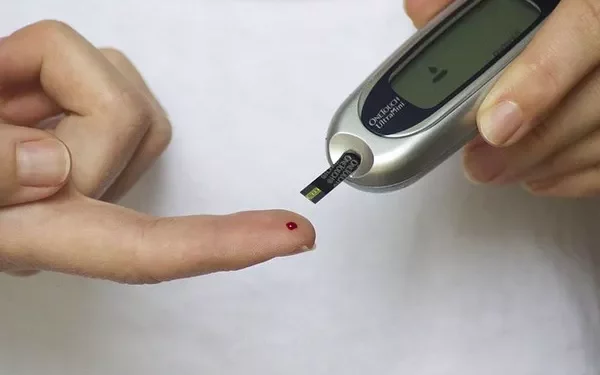
SMBG involves using a blood glucose meter (also known as a glucometer) to measure blood sugar levels. This process typically requires a small blood sample, which is obtained by pricking the finger with a lancet. The blood sample is placed on a test strip, which is inserted into the glucometer. The meter then provides a digital reading of the individual’s blood glucose level.
When to Use SMBG: Most people with diabetes are encouraged to check their blood sugar levels several times a day. The exact frequency depends on factors such as the type of diabetes, medication regimen, and overall health. Typically, testing occurs before or after meals, during periods of exercise, and at bedtime.
Continuous Glucose Monitoring (CGM)
Continuous glucose monitoring (CGM) is a newer technology that provides real-time blood sugar readings throughout the day and night. A small sensor is inserted under the skin (usually on the abdomen or arm) to measure glucose levels in the interstitial fluid (the fluid between cells). The sensor sends data to a receiver or smartphone app, which displays the individual’s glucose trends and alerts them to fluctuations in real time.
When to Use CGM: CGM is especially beneficial for people with type 1 diabetes who require frequent monitoring. It’s also useful for people with type 2 diabetes who experience difficulty managing their blood sugar levels with traditional methods.
The Benefits of Blood Sugar Monitoring for Diabetes
Blood sugar monitoring is not just a diagnostic tool—it’s an essential component of diabetes management. Here are several key benefits of regular blood glucose monitoring for people with diabetes:
1. Better Control of Blood Sugar Levels
One of the most significant benefits of blood sugar monitoring is that it allows individuals to gain better control of their glucose levels. By checking blood sugar regularly, people can track how their levels respond to different foods, medications, and activities. This information allows them to make adjustments to their diet, exercise, and medication regimen to keep blood sugar within a healthy range.
For example:
- If a person notices that their blood sugar rises significantly after consuming a certain type of food, they may decide to reduce or eliminate that food from their diet.
- If blood sugar levels are consistently high before meals, it may indicate the need to adjust insulin doses or oral medications.
2. Early Detection of Blood Sugar Imbalances
Blood sugar levels can fluctuate quickly, and when they become too high (hyperglycemia) or too low (hypoglycemia), they can cause serious health issues. Hyperglycemia can lead to complications such as diabetic ketoacidosis (DKA) in type 1 diabetes or long-term damage to the kidneys, nerves, and blood vessels. On the other hand, hypoglycemia can cause symptoms such as dizziness, confusion, and in severe cases, seizures or unconsciousness.
Frequent monitoring allows individuals to catch these imbalances early, so they can take corrective measures before serious complications arise. For example, if blood sugar levels are dropping too low, individuals can consume a quick source of sugar (such as fruit juice or glucose tablets) to raise their levels before they experience symptoms of hypoglycemia.
3. Personalized Treatment Plan Adjustments
With regular blood sugar readings, individuals can work with their healthcare team to fine-tune their treatment plan. This includes adjusting:
Insulin doses: If blood sugar levels are consistently high, insulin doses may need to be increased, or the type of insulin being used may need to be changed.
Oral medications: Oral medications used in type 2 diabetes (such as metformin or sulfonylureas) may need to be adjusted based on blood sugar patterns.
Diet and exercise: Monitoring blood glucose helps identify which foods or activities have the most significant impact on blood sugar, allowing for more targeted lifestyle changes.
4. Increased Awareness and Empowerment
Regular blood sugar monitoring helps individuals with diabetes become more aware of how their body responds to different factors. This sense of awareness can foster a sense of empowerment, as individuals can actively participate in managing their condition. By understanding the relationship between food, exercise, stress, and blood glucose, individuals can make informed choices that improve their quality of life and reduce the risk of complications.
5. Improved Long-Term Health Outcomes
Studies have shown that tight control of blood glucose levels can help prevent or delay the onset of complications associated with diabetes. Regular blood sugar monitoring is one of the most effective ways to maintain consistent glucose control. By avoiding prolonged periods of high blood sugar (hyperglycemia) and low blood sugar (hypoglycemia), individuals can reduce the risk of complications such as:
Heart disease: Chronic high blood sugar levels increase the risk of heart disease and stroke.
Kidney disease: Consistently high blood sugar can damage the kidneys over time, leading to chronic kidney disease.
Nerve damage: Prolonged high blood sugar levels can cause nerve damage (neuropathy), leading to pain, numbness, and even amputation in severe cases.
Eye disease: High blood sugar levels can damage the blood vessels in the eyes, leading to diabetic retinopathy and blindness.
By monitoring blood sugar closely, individuals can make adjustments to their treatment plan that help lower the risk of these complications.
Different Types of Blood Sugar Monitors
There are several types of blood sugar monitors available, each with its own benefits. The right choice depends on individual preferences, needs, and lifestyle.
1. Traditional Blood Glucose Meters (Glucometers)
Traditional blood glucose meters are portable devices that require a blood sample obtained by pricking the finger. These meters are inexpensive and widely available, making them the most common form of blood sugar monitoring. While they provide an immediate reading, they only offer a snapshot of blood glucose levels at the moment the test is conducted.
2. Continuous Glucose Monitors (CGMs)
CGMs provide real-time glucose data throughout the day and night. They use a small sensor placed under the skin to measure glucose levels in interstitial fluid, and the data is transmitted to a device or smartphone app. CGMs are more expensive than traditional meters, but they provide continuous insights into blood sugar trends, allowing for better proactive management.
3. Flash Glucose Monitors
Flash glucose monitors are similar to CGMs, but they require users to scan the sensor with a device or smartphone to obtain a reading. These monitors provide real-time data but do not continuously transmit data. Flash monitors can be a more affordable option for people who need real-time glucose readings but don’t require constant monitoring.
Challenges of Blood Sugar Monitoring
Despite the numerous benefits of blood sugar monitoring, it’s not without its challenges. Some of the most common barriers to effective monitoring include:
Cost: Blood glucose meters, test strips, and continuous glucose monitors can be expensive, especially if not covered by insurance.
Pain and Inconvenience: Finger pricks, while generally not painful, can become a nuisance for individuals who need to test frequently. CGMs and flash monitors can help reduce the need for finger pricks, but they may still require occasional calibration.
Data Overload: For some individuals, the constant stream of blood glucose data from CGMs can become overwhelming. It’s important to have the support of a healthcare team to interpret this data and make meaningful adjustments.
Conclusion
Blood sugar monitoring is an essential tool for individuals with diabetes. It provides the ability to track glucose levels, make informed decisions about diet, exercise, and medications, and ultimately improve long-term health outcomes. Whether using a traditional glucose meter or a continuous glucose monitor, blood sugar monitoring can help individuals maintain better control over their diabetes, reduce the risk of complications, and lead healthier lives.
Ultimately, the key to effective diabetes management lies in consistency and education. By regularly monitoring blood sugar and working closely with healthcare providers, individuals with diabetes can take charge of their health and manage their condition more effectively.
Related topics:
What Is a Good Estimated Average Glucose Level?