Blood sugar, also known as blood glucose, is an essential metric for understanding metabolic health and is particularly crucial for individuals with diabetes. Blood sugar levels fluctuate throughout the day depending on factors such as diet, activity, stress, and hormonal changes. For those managing diabetes, monitoring these levels is vital to avoid complications and maintain optimal health. But what exactly is considered a normal blood sugar level, and what factors influence these numbers? This article provides an in-depth examination of average blood sugar levels, including how they are measured, what the normal ranges are, and the importance of maintaining healthy glucose levels for both people with and without diabetes.
The Importance of Blood Sugar in Metabolic Health
Glucose is the primary energy source for the body, and blood sugar levels reflect how effectively the body metabolizes this essential fuel. In a healthy person, blood sugar is regulated by the hormone insulin, which allows glucose to enter cells and fuel their activities. However, when this regulation becomes impaired, as in the case of diabetes, blood sugar levels can rise to potentially dangerous levels, leading to various health complications over time, such as cardiovascular disease, nerve damage, kidney issues, and more.
The main types of diabetes—Type 1, Type 2, and gestational diabetes—all involve blood sugar dysregulation. Type 1 diabetes occurs when the pancreas fails to produce sufficient insulin, while Type 2 diabetes is characterized by insulin resistance, meaning the body does not use insulin effectively. Monitoring blood sugar is thus vital for individuals with these conditions, as it allows them to make adjustments to their lifestyle, diet, and medications to keep glucose levels within a healthy range.
How Blood Sugar Levels Are Measured
There are several methods to measure blood sugar levels, each providing valuable insights:
Fasting Blood Sugar (FBS): This test is conducted after an individual has fasted for at least eight hours and provides a baseline measurement. It helps determine if blood glucose levels are normal, prediabetic, or diabetic.
Postprandial Blood Sugar (PPBS): This test measures blood sugar levels two hours after eating. It helps assess how well the body handles sugar intake and is crucial for diagnosing diabetes and understanding post-meal glucose spikes.
Random Blood Sugar (RBS): This test can be done at any time of the day, regardless of when the person last ate. It’s often used in urgent settings to quickly assess glucose levels.
Hemoglobin A1C (HbA1c): This test measures average blood sugar levels over the past two to three months by assessing the percentage of glycated hemoglobin in the blood. It’s particularly valuable for long-term monitoring and is used to assess the effectiveness of diabetes management.
Each test offers a different snapshot of blood sugar regulation, and together, they provide a comprehensive view of an individual’s glucose metabolism.
Normal Blood Sugar Levels: Fasting, Post-Meal, and A1C Ranges
Blood sugar levels vary depending on the context in which they are measured. Below are the standard ranges used by healthcare professionals to evaluate whether blood glucose is within normal limits:
Fasting Blood Sugar Levels
Normal: 70-99 mg/dL (3.9-5.5 mmol/L)
Prediabetes: 100-125 mg/dL (5.6-6.9 mmol/L)
Diabetes: 126 mg/dL (7.0 mmol/L) or higher on two separate tests
Fasting blood sugar provides a baseline for understanding how well the body maintains glucose levels without the influence of recent food intake. For individuals with diabetes, maintaining fasting blood glucose within a controlled range is essential to avoid the risk of chronic complications.
Postprandial Blood Sugar Levels (Two Hours After a Meal)
Normal: Less than 140 mg/dL (7.8 mmol/L)
Prediabetes: 140-199 mg/dL (7.8-11.0 mmol/L)
Diabetes: 200 mg/dL (11.1 mmol/L) or higher
Post-meal blood sugar levels give insights into how the body manages glucose after food intake. Elevated postprandial levels are a common issue in individuals with Type 2 diabetes, where insulin resistance may prevent cells from effectively utilizing glucose.
Hemoglobin A1C (HbA1c) Levels
Normal: Below 5.7%
Prediabetes: 5.7%-6.4%
Diabetes: 6.5% or higher
The HbA1c test is unique because it provides a long-term picture of blood sugar levels. Unlike fasting or post-meal tests, which reflect glucose levels at specific times, HbA1c reflects average blood glucose over two to three months. This makes it an excellent marker for monitoring the effectiveness of diabetes management and assessing the risk of complications.
Factors Influencing Blood Sugar Levels
Blood sugar levels are influenced by various lifestyle, physiological, and environmental factors. Understanding these factors can help individuals manage their glucose levels more effectively.
Diet and Carbohydrate Intake
Carbohydrates have the most significant impact on blood sugar levels, as they are broken down into glucose during digestion. Foods with a high glycemic index (GI) lead to rapid blood sugar spikes, while those with a low GI have a slower, more moderate effect. For example, refined grains and sugary snacks tend to elevate blood sugar quickly, whereas complex carbohydrates like whole grains, legumes, and vegetables result in a slower release of glucose.
Physical Activity
Physical activity helps lower blood sugar levels by increasing insulin sensitivity, allowing cells to use glucose more efficiently. Regular exercise is especially beneficial for individuals with diabetes, as it can help lower fasting blood glucose, reduce insulin resistance, and promote weight loss.
Sleep and Stress
Both sleep quality and stress levels can impact blood sugar. Chronic sleep deprivation can lead to insulin resistance, while stress triggers the release of hormones like cortisol and adrenaline, which can elevate blood sugar levels. Managing stress through techniques such as meditation, yoga, and adequate rest is therefore crucial for blood sugar control.
Hormonal Changes
Hormones can also play a role in blood sugar fluctuations. For example, during periods of growth, pregnancy, or menopause, hormonal changes can affect insulin sensitivity and lead to higher blood sugar levels. This is particularly notable for women, as menstrual cycles and hormonal changes related to menopause can create additional challenges in blood sugar management.
Medications
Certain medications, such as corticosteroids, birth control pills, and some antipsychotic drugs, can raise blood sugar levels. Individuals with diabetes should consult with their healthcare provider when taking new medications to assess their impact on blood sugar levels.
Blood Sugar Targets for Different Populations
Blood sugar targets may vary depending on an individual’s age, health status, and diabetes management goals. Here are some general guidelines for different groups:
Children and Adolescents with Diabetes
Managing diabetes in children and adolescents requires special considerations due to growth and developmental needs. Blood sugar targets are often set slightly higher than for adults to reduce the risk of hypoglycemia (low blood sugar).
Fasting: 80-130 mg/dL
Post-meal: Less than 180 mg/dL
HbA1c: Less than 7.5%
Adults with Diabetes
For adults with diabetes, blood sugar targets depend on factors such as age, duration of diabetes, and presence of complications. Maintaining glucose within target ranges helps reduce the risk of complications.
Fasting: 80-130 mg/dL
Post-meal: Less than 180 mg/dL
HbA1c: Less than 7.0%
Older Adults with Diabetes
In older adults, blood sugar targets may be slightly higher, especially if there are other health issues or a risk of hypoglycemia. The focus is on maintaining quality of life and avoiding hypoglycemia.
Fasting: 90-150 mg/dL
Post-meal: Less than 200 mg/dL
HbA1c: Less than 8.0%
The Importance of Consistent Blood Sugar Monitoring
Regular blood sugar monitoring is key to managing diabetes effectively. The frequency and method of monitoring will depend on individual needs and the type of diabetes. Individuals with Type 1 diabetes, for example, may need to check their blood sugar multiple times a day, while those with Type 2 diabetes may monitor less frequently.
Continuous Glucose Monitoring (CGM)
CGM devices provide real-time data on blood sugar levels, allowing individuals to track trends and make timely adjustments to their diet, physical activity, or medication. These devices are particularly useful for those who experience frequent fluctuations or have difficulty identifying symptoms of low or high blood sugar.
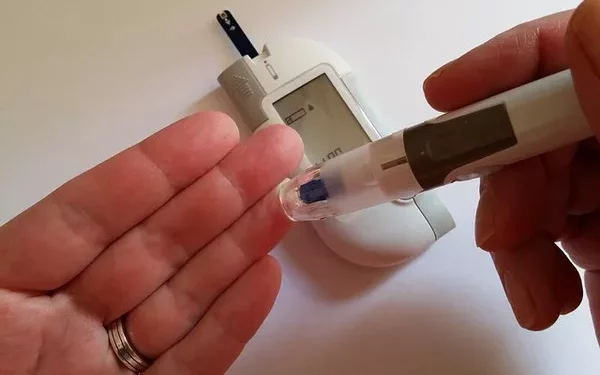
Fingerstick Testing
Traditional fingerstick testing remains a reliable method for monitoring blood sugar, particularly for those who may not have access to CGM. While this method provides single-point data, it can still be effective when done regularly and at specific times, such as before meals, after meals, and at bedtime.
Achieving and Maintaining Optimal Blood Sugar Levels
Maintaining blood sugar within the normal range involves a combination of diet, exercise, and, if necessary, medication. Here are some strategies that can help achieve optimal blood glucose levels:
Balanced Diet: Focus on whole foods with a low glycemic index, such as vegetables, whole grains, and lean proteins. Avoiding sugary foods and refined carbohydrates can help stabilize blood sugar.
Regular Exercise: Engage in physical activity at least five days a week. A mix of aerobic and resistance exercises is beneficial for improving insulin sensitivity.
Adequate Sleep: Aim for 7-9 hours of quality sleep each night to reduce the risk of insulin resistance and promote metabolic health.
Stress Management: Use techniques like meditation, deep breathing, or yoga to manage stress, which can contribute to blood sugar fluctuations.
Medication Adherence: If prescribed, it’s essential to take diabetes medications as directed and consult with a healthcare provider about any concerns.
Conclusion
Average blood sugar levels provide a critical benchmark for understanding metabolic health, especially for individuals with diabetes. Knowing what constitutes normal fasting, post-meal, and long-term blood sugar levels can help in assessing one’s risk for diabetes-related complications. With regular monitoring and a proactive approach to lifestyle management, individuals can significantly improve their blood sugar control, reduce the risk of complications, and enjoy a better quality of life.
Achieving stable blood sugar is not only about numbers but about maintaining overall health and wellness. By following the recommended strategies and working closely with healthcare providers, those with diabetes can take control of their blood sugar levels and improve their long-term outcomes.
Related topics:
What Should Be Normal Diabetes