Diabetes is a chronic condition that affects millions of people worldwide, characterized by abnormal blood sugar (glucose) levels. Maintaining blood glucose within a normal range is essential for managing diabetes and preventing complications. However, what is considered “normal” when it comes to blood glucose levels? The concept of “normal” diabetes involves understanding the various blood glucose targets that differ based on factors such as type of diabetes, time of day, and recent meals.
In this article, we will explore what constitutes normal blood glucose levels, the importance of monitoring these levels regularly, and how to interpret blood glucose readings for optimal diabetes management.
Understanding Blood Glucose and Its Role in the Body
Blood glucose, or blood sugar, refers to the concentration of glucose in the bloodstream. Glucose is a simple sugar that comes from the breakdown of carbohydrates in food and is the body’s primary source of energy. The body regulates blood glucose levels through the hormone insulin, produced by the pancreas. Insulin helps cells absorb glucose from the blood, thus maintaining a stable blood sugar level.
When blood glucose levels become too high or too low, it can lead to serious health problems. For individuals with diabetes, the body either does not produce enough insulin (type 1 diabetes) or does not respond properly to insulin (type 2 diabetes), leading to impaired blood glucose regulation.
The goal of diabetes management is to maintain blood glucose levels within a target range to avoid complications such as nerve damage, cardiovascular disease, and kidney problems. The concept of “normal” blood glucose levels is essential in managing these risks.
What Are Normal Blood Glucose Levels?
The definition of “normal” blood glucose levels varies depending on the individual, the time of day, and whether or not the person has diabetes. To provide clarity, blood glucose levels are generally categorized based on two types of measurements: fasting glucose levels and post-meal (postprandial) glucose levels. These readings can be taken through self-monitoring of blood glucose (SMBG) or by using a continuous glucose monitor (CGM).
Fasting Blood Glucose (FBG) Levels
Fasting blood glucose levels are measured after an individual has not eaten for at least eight hours (typically overnight). This is a common measure to assess glucose regulation and is often used as a diagnostic tool for diabetes.
Normal Fasting Blood Glucose: A fasting blood glucose level of 70–99 mg/dL (3.9–5.5 mmol/L) is considered normal.
Prediabetes Fasting Blood Glucose: A fasting blood glucose level of 100–125 mg/dL (5.6–6.9 mmol/L) indicates prediabetes, a condition where blood sugar levels are higher than normal but not yet high enough to be classified as diabetes.
Diabetes Fasting Blood Glucose: A fasting blood glucose level of 126 mg/dL (7.0 mmol/L) or higher on two separate occasions suggests diabetes.
Postprandial Blood Glucose Levels
Postprandial blood glucose refers to blood glucose levels measured 1–2 hours after eating. After consuming a meal, blood sugar levels rise, but they should return to baseline levels within a few hours.
Normal Postprandial Blood Glucose: Blood glucose levels should be less than 140 mg/dL (7.8 mmol/L) 2 hours after eating for someone without diabetes.
Prediabetes Postprandial Blood Glucose: Blood glucose levels of 140–199 mg/dL (7.8–11.0 mmol/L) after meals may indicate prediabetes.
Diabetes Postprandial Blood Glucose: Blood glucose levels of 200 mg/dL (11.1 mmol/L) or higher after meals are consistent with diabetes.
A1C (Glycated Hemoglobin) Levels
The A1C test measures the percentage of hemoglobin in the blood that is coated with sugar (glycated), reflecting average blood glucose levels over the past 2–3 months. It is commonly used to assess long-term blood glucose control.
Normal A1C Levels: An A1C of less than 5.7% is considered normal.
Prediabetes A1C Levels: An A1C between 5.7% and 6.4% indicates prediabetes.
Diabetes A1C Levels: An A1C of 6.5% or higher is diagnostic of diabetes.
Random Blood Glucose Levels
Random blood glucose levels are measured at any time of day, regardless of when the person last ate. It is often used as a preliminary screening for diabetes.
Normal Random Blood Glucose: A normal random blood glucose level is less than 140 mg/dL (7.8 mmol/L).
Diabetes Random Blood Glucose: A random blood glucose level of 200 mg/dL (11.1 mmol/L) or higher, along with symptoms of diabetes such as excessive thirst or frequent urination, can indicate diabetes.
Blood Glucose Targets for People with Diabetes
For individuals diagnosed with diabetes, the target blood glucose levels may be different from those considered “normal.” The goal is to keep blood sugar levels within a range that minimizes the risk of complications without being too strict, which could lead to hypoglycemia (low blood sugar).
The American Diabetes Association (ADA) recommends the following blood glucose targets for most adults with diabetes:
Fasting Blood Glucose: 80–130 mg/dL (4.4–7.2 mmol/L)
Postprandial Blood Glucose: Less than 180 mg/dL (10.0 mmol/L) 1–2 hours after meals
A1C: Less than 7% for most people with diabetes
These targets may vary based on individual circumstances, such as age, duration of diabetes, overall health, and risk of hypoglycemia. It is essential for individuals with diabetes to work with their healthcare providers to determine personalized blood glucose targets.
Factors Affecting Blood Glucose Levels
Several factors can influence blood glucose levels, even in people without diabetes. Understanding these factors is crucial for managing blood glucose and maintaining normal ranges.
Diet
Dietary choices play a significant role in blood glucose regulation. Consuming a balanced diet with healthy carbohydrates, lean proteins, and healthy fats can help maintain stable blood glucose levels. For example:
- High-fiber foods, such as vegetables, legumes, and whole grains, can slow the absorption of glucose and help prevent blood sugar spikes.
- Simple carbohydrates, such as sugary snacks, refined grains, and sugary drinks, can cause rapid increases in blood sugar levels.
Physical Activity
Exercise helps the body use glucose more efficiently, lowering blood sugar levels. Regular physical activity improves insulin sensitivity, making it easier for the body to regulate blood glucose levels. Both aerobic exercises (e.g., walking, running) and strength training (e.g., weightlifting) can contribute to better blood glucose control.
Medications
For individuals with diabetes, medications may be required to help regulate blood glucose. Insulin and oral medications, such as metformin, sulfonylureas, and GLP-1 receptor agonists, can help lower blood sugar levels. These medications can affect blood glucose levels in different ways, and it’s important for individuals to monitor their glucose regularly to ensure they are within the target range.
Stress
Chronic stress can lead to elevated blood glucose levels due to the release of stress hormones like cortisol. Managing stress through relaxation techniques such as meditation, yoga, or deep breathing exercises can help maintain normal blood sugar levels.
Illness
When the body is fighting an illness or infection, blood glucose levels can rise. Illness causes the body to release stress hormones, which can lead to insulin resistance. Monitoring blood glucose levels closely during illness is important to avoid complications.
Sleep
Poor sleep or sleep disorders can affect insulin sensitivity and blood glucose control. Aim for 7–9 hours of sleep per night to promote optimal blood sugar regulation.
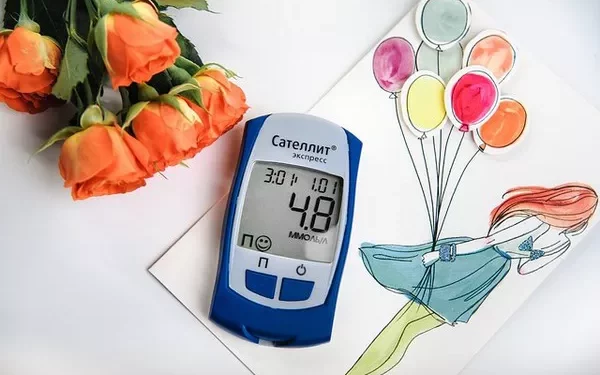
The Importance of Regular Blood Glucose Monitoring
Regular blood glucose monitoring is crucial for individuals with diabetes to keep their blood sugar levels within a normal or target range. Self-monitoring of blood glucose (SMBG) allows individuals to check their blood sugar levels at different times throughout the day, including before and after meals, and to adjust their diet, exercise, and medications accordingly.
Continuous glucose monitoring (CGM) is another option that provides real-time blood glucose readings throughout the day and night, offering greater insights into fluctuations in blood sugar. Both SMBG and CGM help identify patterns, such as post-meal blood sugar spikes, and help individuals make informed decisions about their diabetes management.
Conclusion
Normal blood glucose levels are essential for overall health, particularly for individuals with diabetes. Understanding the target ranges for fasting blood glucose, postprandial glucose, A1C, and random blood glucose is critical for managing diabetes and preventing complications. Regular blood glucose monitoring, along with proper diet, exercise, medication, and lifestyle management, is the cornerstone of diabetes care.
Individuals with diabetes should work closely with their healthcare team to develop a personalized diabetes management plan that includes regular monitoring, healthy lifestyle choices, and medication as needed. By staying within the recommended target blood glucose levels, individuals can significantly reduce their risk of complications and live healthier, more fulfilling lives.
Related topics: